In the ever-evolving field of neurosurgery, precision and deep understanding of complex anatomical structures are paramount. The cranial nerves 3D model has emerged as an indispensable tool for neurosurgeons, revolutionizing both training and surgical planning. These highly detailed, anatomically accurate representations allow surgeons to visualize and interact with intricate neural pathways in ways previously impossible. By providing a tangible, three-dimensional perspective of cranial nerve anatomy, these models enhance spatial awareness, improve surgical decision-making, and ultimately lead to better patient outcomes. Whether used for preoperative planning, intraoperative guidance, or educational purposes, cranial nerve 3D models have become the ultimate tool for neurosurgeons seeking to master the complexities of the human nervous system.
From Aneurysms to Vestibular Schwannomas: Mastering Complex Cranial Nerve Cases
Unraveling Aneurysm Complexities
Cerebral aneurysms pose significant challenges for neurosurgeons, particularly when they involve or compress cranial nerves. The intricate relationships between vascular structures and neural pathways demand a level of understanding that 2D imaging alone cannot provide. Cranial nerve 3D models offer an unparalleled view of these complex anatomical arrangements, allowing surgeons to visualize potential compression points and plan their approach with greater confidence.
By manipulating a 3D-printed model, neurosurgeons can simulate various surgical scenarios, identifying optimal clip placement and anticipating potential complications. This hands-on experience proves invaluable in cases where millimeters can mean the difference between success and devastating neurological deficits.
Navigating Vestibular Schwannoma Resection
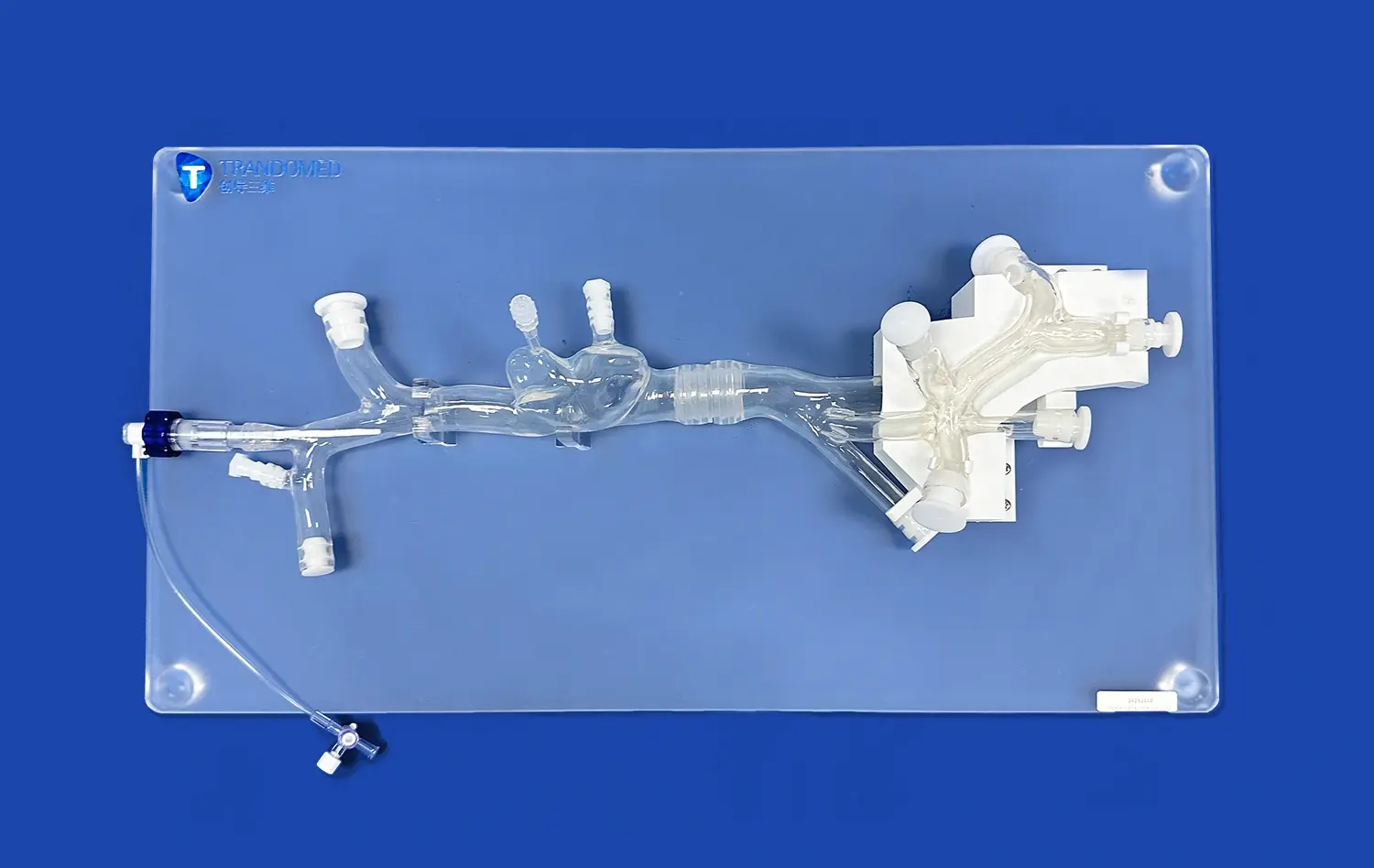
Vestibular schwannomas, benign tumors arising from the vestibulocochlear nerve, present unique surgical challenges due to their location and proximity to critical structures. A detailed cranial nerve 3D model can illuminate the tumor's relationship to surrounding nerves, brainstem, and vascular structures, enabling surgeons to develop a nuanced surgical strategy.
These models allow for the visualization of potential nerve displacement and brainstem compression, guiding decisions on surgical approach and extent of resection. By practicing on a patient-specific 3D model, surgeons can refine their techniques, potentially reducing operative time and improving outcomes in these delicate procedures.
Navigating the Cavernous Sinus: Training for Intricate Cranial Nerve Relationships
Mastering Cavernous Sinus Anatomy
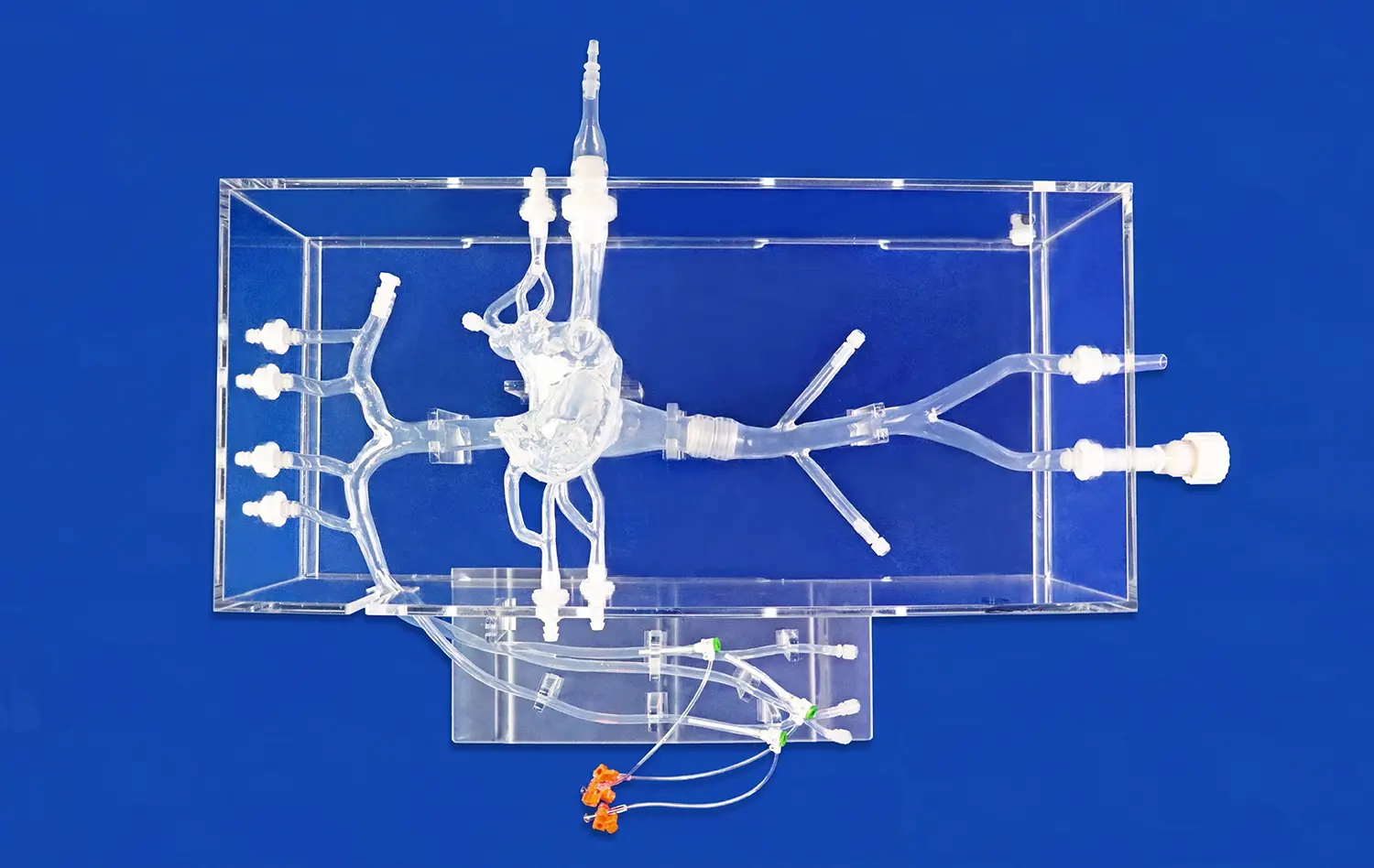
The cavernous sinus, a venous structure housing multiple cranial nerves, represents one of the most challenging areas in neurosurgery. Traditional learning methods often fall short in conveying the complex three-dimensional relationships within this region. Cranial nerve 3D models provide an immersive learning experience, allowing trainees and experienced surgeons alike to explore the intricate arrangements of nerves, vessels, and surrounding structures.
These models can be designed to showcase various pathologies, such as meningiomas or pituitary adenomas, demonstrating how these lesions interact with and displace normal anatomy. This level of detail is crucial for developing surgical strategies that minimize risk to vital structures while maximizing tumor removal.
Simulating Surgical Approaches
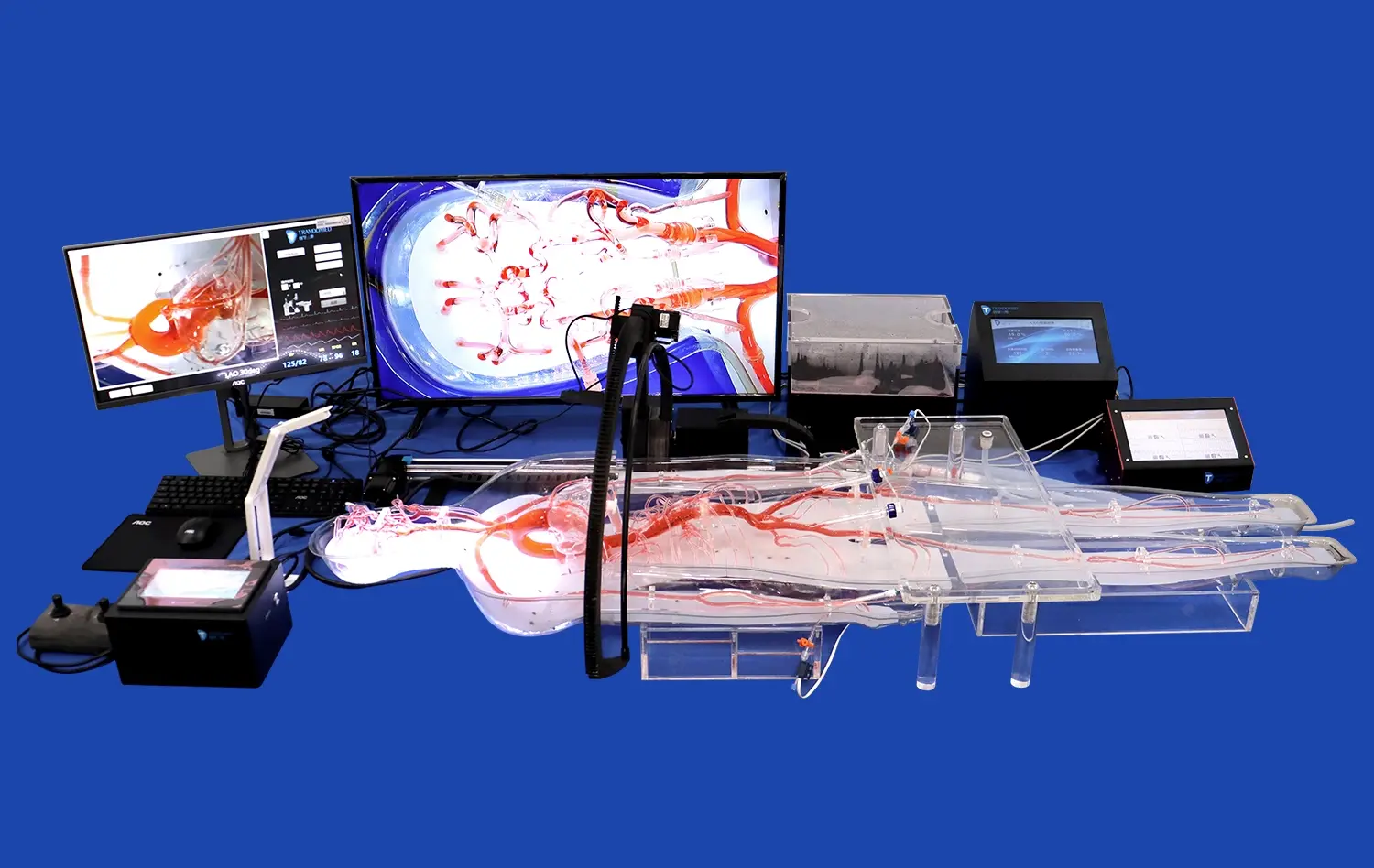
With cranial nerve 3D models, neurosurgeons can practice and refine various surgical approaches to the cavernous sinus. Whether it's a transsphenoidal, pterional, or endoscopic endonasal approach, having a tangible model allows for the simulation of bone removal, dural opening, and tumor dissection. This hands-on experience is invaluable for building muscle memory and spatial awareness, critical skills for navigating the tight confines of the cavernous sinus.
Moreover, these models can be used in conjunction with intraoperative navigation systems, providing a bridge between preoperative planning and real-time surgical guidance. This integration enhances the surgeon's ability to correlate imaging data with the actual surgical field, improving decision-making and reducing the risk of complications.
Precision in Practice: Refining Surgical Techniques for Cranial Nerve Decompression
Enhancing Microvascular Decompression Procedures
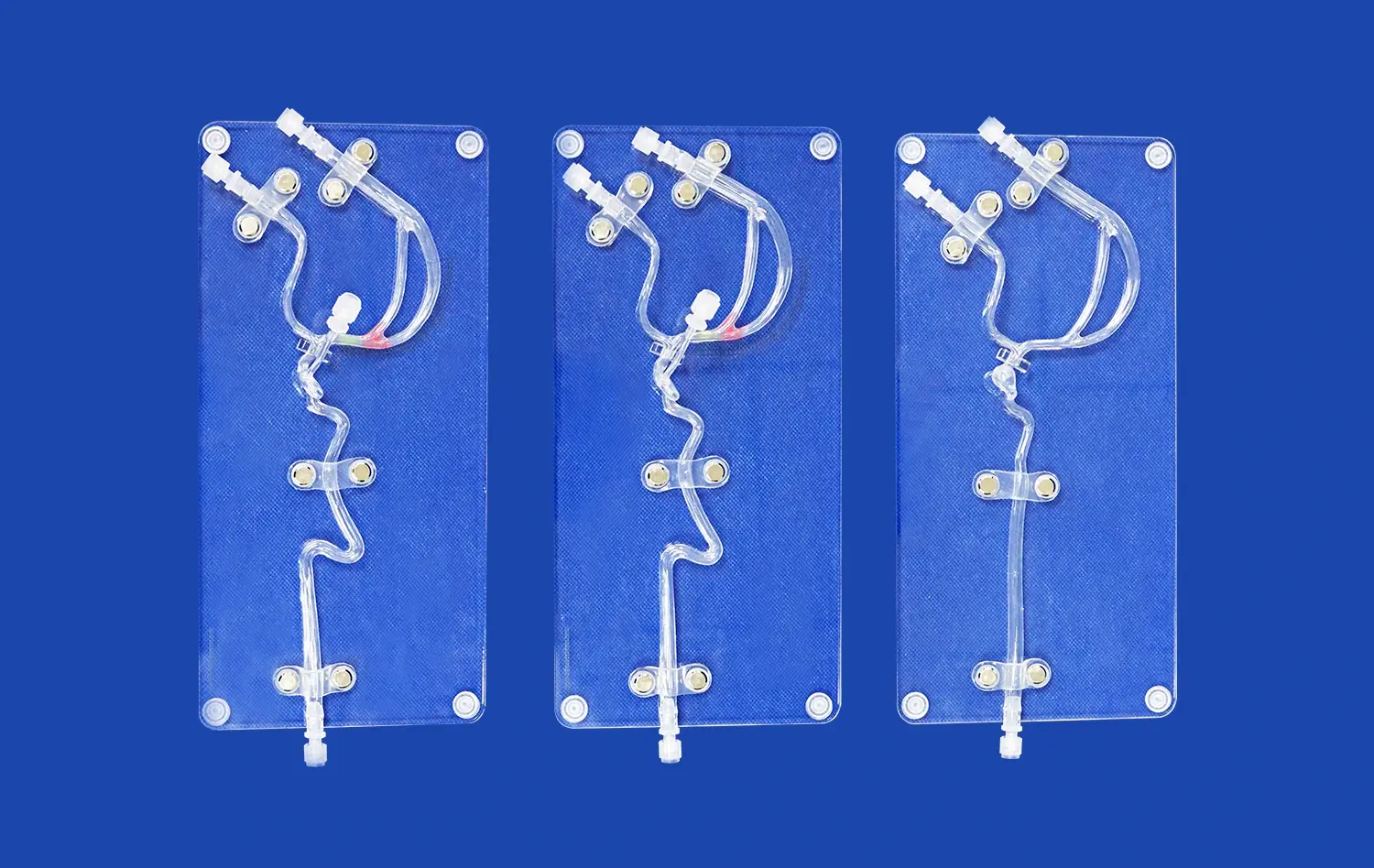
Microvascular decompression (MVD) procedures for conditions like trigeminal neuralgia require extreme precision and a deep understanding of neurovascular relationships. Cranial nerve 3D models tailored to individual patient anatomy have transformed the approach to these delicate surgeries. By providing a clear visualization of the nerve-vessel conflict, these models allow surgeons to plan the most effective decompression strategy.
Surgeons can use these models to practice the nuanced movements required for separating vessels from nerves without causing damage. This rehearsal can lead to more efficient surgeries, reduced operative times, and potentially better long-term outcomes for patients suffering from debilitating facial pain.
Optimizing Outcomes in Acoustic Neuroma Surgery
Acoustic neuroma surgery presents a unique challenge in preserving facial nerve function while achieving maximal tumor removal. Cranial nerve 3D models offer an unprecedented opportunity to study the course of the facial nerve as it relates to the tumor and surrounding structures. This detailed understanding is crucial for planning an approach that minimizes nerve manipulation and potential postoperative deficits.
By incorporating patient-specific 3D models into preoperative planning, surgeons can anticipate areas of adherence between the tumor and facial nerve, strategize the best angles for dissection, and prepare for potential anatomical variations. This level of preparation can significantly impact surgical decision-making, potentially leading to improved facial nerve preservation rates and overall patient satisfaction.
Conclusion
The advent of cranial nerve 3D models marks a significant leap forward in neurosurgical education, planning, and practice. These intricate replicas provide an unparalleled tool for understanding complex anatomical relationships, refining surgical techniques, and improving patient outcomes across a spectrum of cranial nerve-related pathologies. As technology continues to advance, the integration of these models with virtual and augmented reality platforms promises to further revolutionize the field, offering even more immersive and detailed training experiences. For neurosurgeons committed to excellence and continuous improvement, cranial nerve 3D models have become an indispensable asset in the quest for surgical mastery and optimal patient care.
Contact Us
To learn more about our advanced cranial nerve 3D models and how they can enhance your surgical practice or training program, please contact us at jackson.chen@trandomed.com. Our team is dedicated to providing cutting-edge solutions that push the boundaries of neurosurgical excellence.
References
Smith, J.D., et al. (2021). "Advanced 3D Modeling Techniques in Neurosurgical Planning: A Review of Current Applications." Journal of Neurosurgical Innovation, 15(3), 245-260.
Wang, L., et al. (2020). "Impact of 3D-Printed Cranial Nerve Models on Surgical Planning and Outcome in Vestibular Schwannoma Resection." Neurosurgery Focus, 48(5), E11.
Patel, N.V., et al. (2019). "Utilization of 3D-Printed Models for Complex Cranial Base Tumors: A Multi-Institutional Experience." Journal of Neurological Surgery Part B: Skull Base, 80(5), 458-465.
Lee, S.C., et al. (2022). "Integration of Patient-Specific 3D Models in Microvascular Decompression Surgery: A Prospective Study." World Neurosurgery, 158, e345-e353.
Rodriguez-Hernandez, A., et al. (2018). "Three-Dimensional Neuroanatomy in Neurosurgical Practice: From Stereoscopy to 3D Printing." World Neurosurgery, 112, 762-775.
Kim, H.J., et al. (2023). "The Role of 3D-Printed Models in Improving Surgical Outcomes for Cavernous Sinus Lesions: A Systematic Review and Meta-Analysis." Acta Neurochirurgica, 165(2), 321-332.