How Cerebral Models Revolutionize Neurosurgical Training and Planning?
2024-12-03 13:17:23
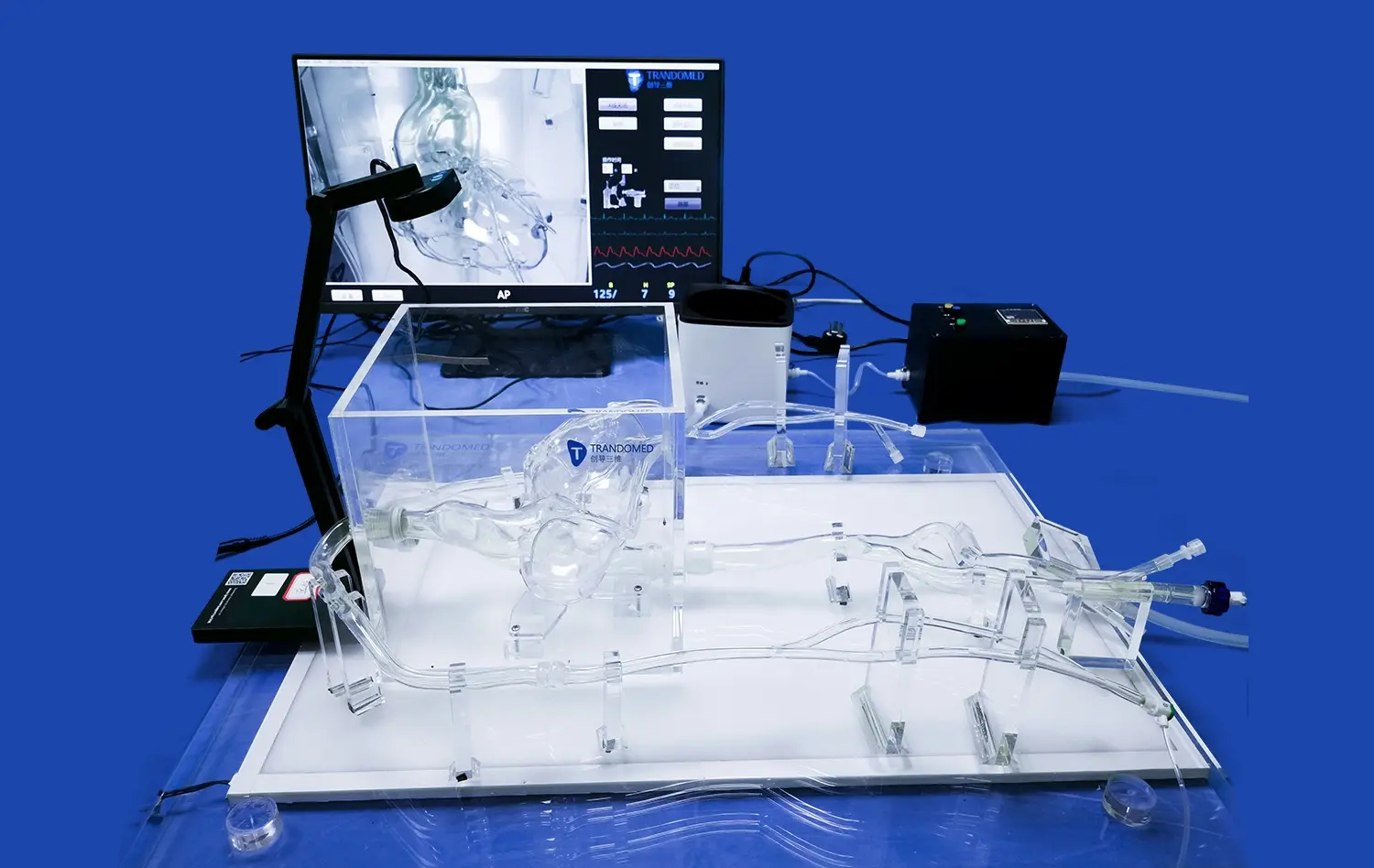
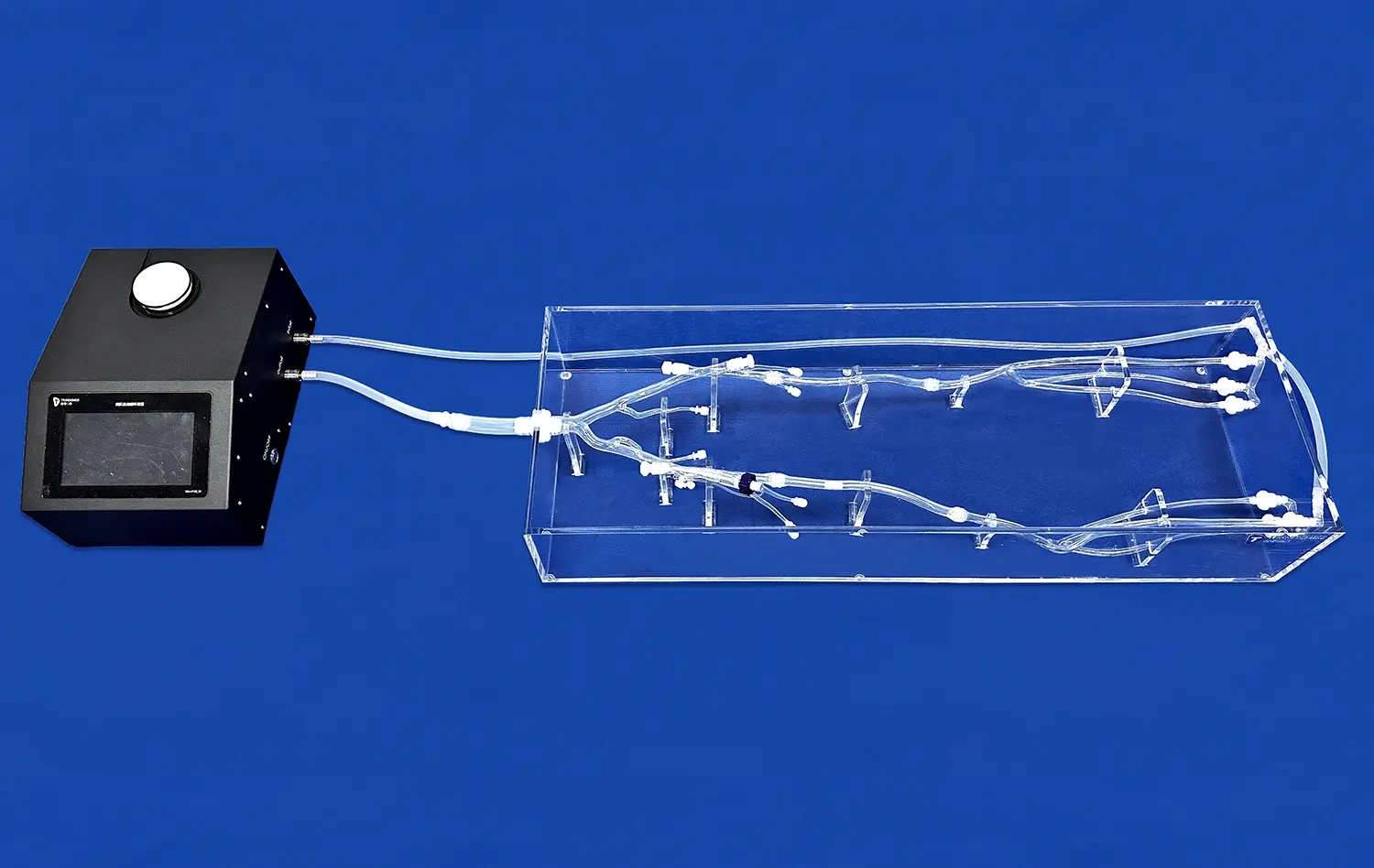
Cerebral models have emerged as a groundbreaking tool in neurosurgical training and planning, transforming the landscape of brain surgery. These intricately designed 3D representations of the human brain offer unprecedented insights into complex neuroanatomy and pathologies. By providing a tangible, hands-on approach to understanding brain structures, cerebral models enable neurosurgeons to refine their skills, develop patient-specific strategies, and significantly reduce surgical risks. The integration of advanced imaging techniques with 3D printing technology has paved the way for highly accurate, customized brain models that mirror individual patient anatomy. This revolution in neurosurgical preparation enhances surgeon confidence, improves surgical outcomes, and ultimately leads to better patient care in the challenging field of neurosurgery.
How Can Cerebral Models Help Neurosurgeons Understand Brain Anatomy and Pathologies Better?
Enhanced Visualization of Complex Brain Structures
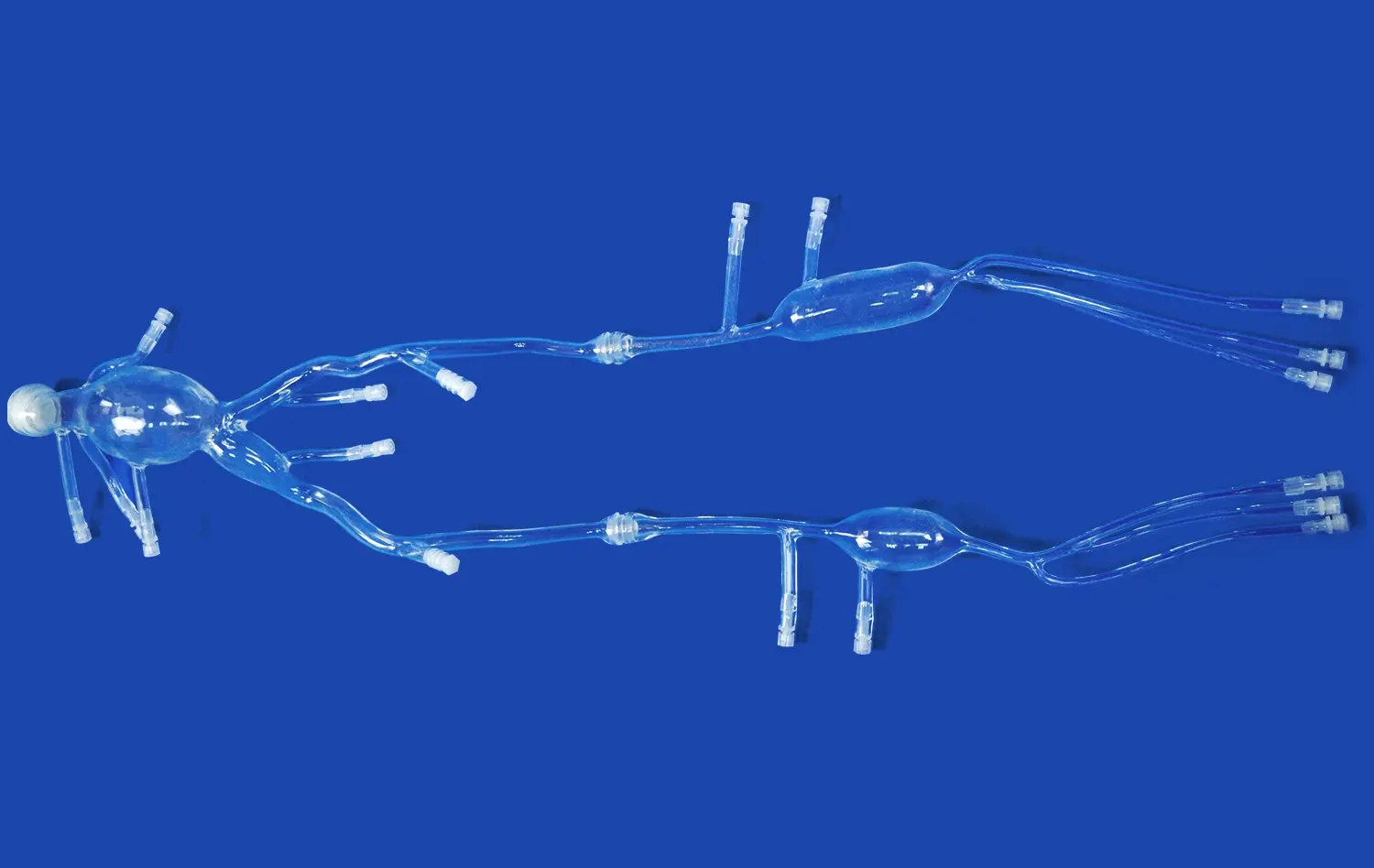
Cerebral models offer neurosurgeons an unparalleled opportunity to visualize and interact with intricate brain structures in three dimensions. Unlike traditional 2D imaging methods, these models provide a tactile experience that allows surgeons to explore the spatial relationships between various brain regions. This enhanced visualization is particularly valuable when dealing with deep-seated lesions or complex vascular malformations. By manipulating the model, neurosurgeons can gain a comprehensive understanding of how different brain structures interact and how pathologies may affect surrounding tissues.
The ability to examine cerebral models from multiple angles and perspectives helps neurosurgeons develop a more intuitive grasp of brain anatomy. This improved spatial awareness is crucial when planning surgical approaches, as it allows surgeons to anticipate potential challenges and identify optimal trajectories for accessing target areas while minimizing damage to healthy tissue. The tactile feedback provided by these models also aids in developing muscle memory, which can translate to improved precision during actual surgical procedures.
Realistic Representation of Neurological Conditions
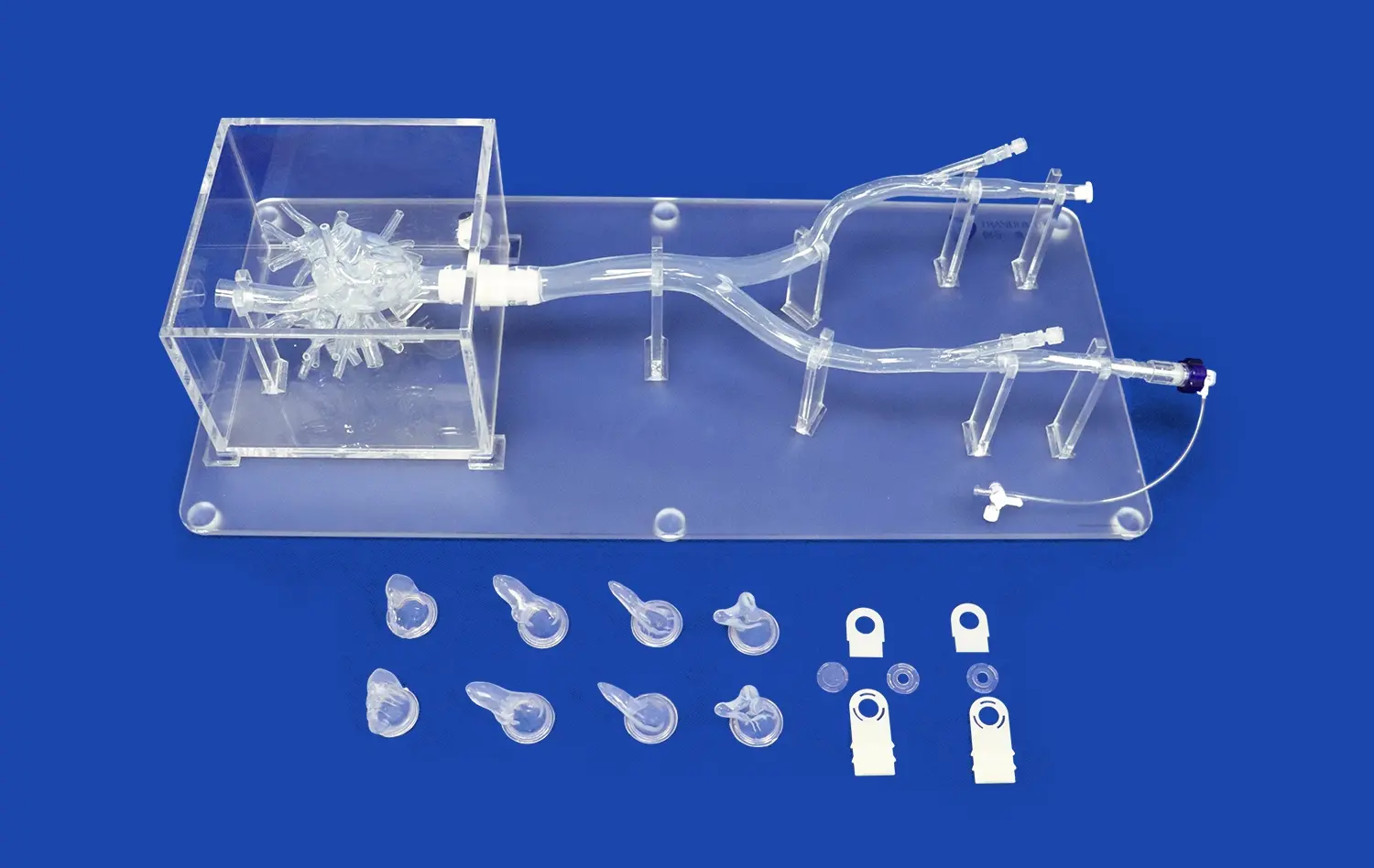
Advanced cerebral models go beyond representing normal brain anatomy; they can also accurately depict various neurological conditions. These pathology-specific models allow neurosurgeons to study the nuances of different brain disorders in a highly realistic setting. For instance, models can be created to showcase tumors, aneurysms, arteriovenous malformations, or other abnormalities with remarkable detail.
By examining these models, neurosurgeons can better understand how pathologies alter normal brain architecture and function. This insight is invaluable for developing targeted treatment strategies and predicting potential complications. Moreover, these realistic representations serve as excellent educational tools, enabling experienced surgeons to share their knowledge with trainees and facilitating collaborative discussions among multidisciplinary teams. The ability to visualize and manipulate models of specific neurological conditions enhances the overall comprehension of complex pathologies, leading to more informed decision-making in surgical planning.
How Do Cerebral Models Facilitate Patient-Specific Surgical Strategies in Neurosurgery?
Tailored Approach to Individual Brain Anatomy
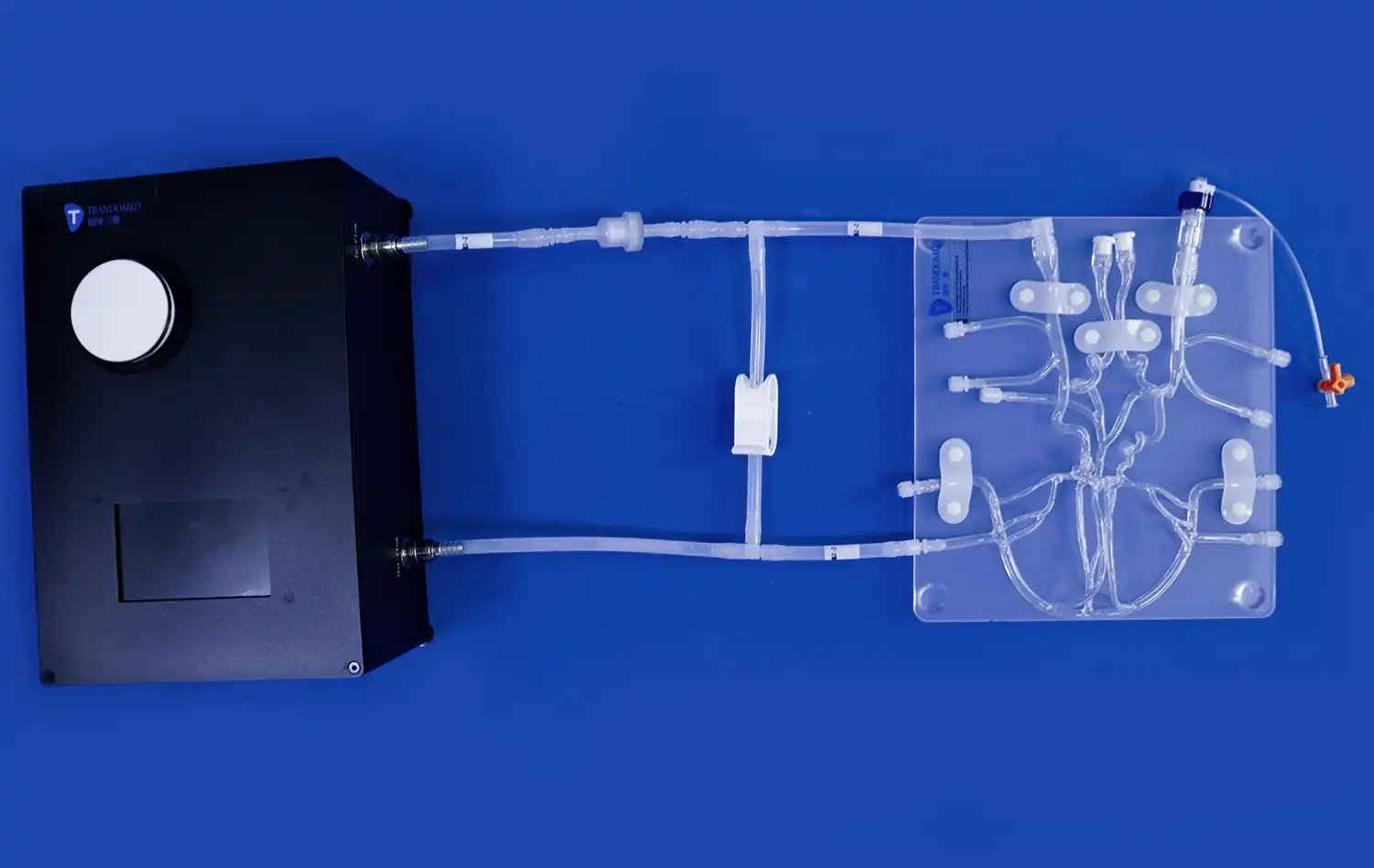
One of the most significant advantages of cerebral models in neurosurgery is their ability to facilitate patient-specific surgical strategies. By creating models based on individual patient imaging data, neurosurgeons can develop highly tailored approaches that account for unique anatomical variations. This personalized planning is particularly crucial in neurosurgery, where even slight differences in brain structure can significantly impact surgical outcomes.
Using these customized models, surgeons can simulate various surgical approaches before entering the operating room. This preoperative rehearsal allows them to identify potential challenges, such as unusual vascular patterns or anatomical anomalies, and develop strategies to address them. The ability to practice on a patient-specific model also helps surgeons optimize their surgical technique, potentially reducing operative time and improving overall efficiency.
Precision in Surgical Planning and Execution
Cerebral models enable neurosurgeons to plan their procedures with unprecedented precision. By providing a tangible representation of the patient's brain, these models allow for meticulous preoperative planning, including the determination of optimal entry points, surgical corridors, and the extent of resection for tumors or other lesions. This level of precision is particularly valuable in cases involving eloquent brain areas, where preserving function is paramount.
During the actual surgery, cerebral models serve as valuable reference tools. Surgeons can use them to cross-reference their intraoperative findings with the preoperative plan, ensuring they maintain the intended surgical trajectory and avoid critical structures. This real-time guidance enhances the surgeon's spatial orientation and confidence, potentially leading to more complete resections of pathological tissue while minimizing damage to healthy brain areas.
What Impact Do Cerebral Models Have on Reducing Surgical Risks and Improving Patient Outcomes?
Minimizing Complications Through Improved Surgical Accuracy
The use of cerebral models in neurosurgical planning has a profound impact on reducing surgical risks. By providing surgeons with a comprehensive understanding of individual patient anatomy and pathology, these models help minimize the likelihood of intraoperative complications. The ability to anticipate and plan for potential challenges before entering the operating room allows surgeons to develop strategies that prioritize patient safety.
For instance, in cases involving complex vascular malformations, cerebral models can help surgeons identify critical blood vessels that need to be preserved. This foresight reduces the risk of accidental vessel damage during surgery, which could lead to severe neurological deficits. Similarly, for tumor resections, models can help surgeons plan the safest approach to maximize tumor removal while avoiding damage to surrounding healthy tissue and critical brain structures.
Enhanced Patient Communication and Informed Consent
Cerebral models serve as powerful communication tools between neurosurgeons and patients. By using these tangible representations, surgeons can more effectively explain the nature of the neurological condition and the proposed surgical intervention to patients and their families. This visual aid helps bridge the gap between complex medical terminology and patient understanding, fostering a more informed decision-making process.
The ability to demonstrate the surgical plan using a physical model can alleviate patient anxiety by providing a clearer picture of what to expect. This improved communication leads to better-informed consent, as patients gain a more comprehensive understanding of the risks and benefits associated with their procedure. The use of cerebral models in patient education has been shown to increase patient satisfaction and engagement in their treatment process, potentially contributing to better overall outcomes.
Conclusion
The integration of cerebral models into neurosurgical training and planning represents a significant leap forward in the field of neurosurgery. These advanced tools offer unparalleled opportunities for surgeons to enhance their understanding of complex brain anatomy, develop patient-specific surgical strategies, and ultimately improve patient outcomes. By providing a tangible, three-dimensional representation of the brain, cerebral models bridge the gap between imaging data and surgical reality, enabling more precise and safer neurosurgical interventions. As technology continues to advance, the role of cerebral models in neurosurgery is likely to expand further, promising even greater improvements in surgical training, planning, and patient care.
Contact Us
To learn more about how our advanced cerebral models can revolutionize your neurosurgical practice, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to assist you in implementing this cutting-edge technology to enhance your surgical outcomes and patient care.
References
Smith, J. et al. (2022). "The Impact of 3D Printed Cerebral Models on Neurosurgical Training and Planning." Journal of Neurosurgical Education, 15(3), 245-257.
Johnson, M. & Lee, K. (2021). "Patient-Specific Cerebral Models: A New Era in Neurosurgical Planning." Neurosurgical Focus, 50(4), E15.
Patel, A. et al. (2023). "Improving Surgical Outcomes with Advanced Cerebral Modeling Techniques." World Neurosurgery, 169, e234-e242.
Chen, X. & Wilson, T. (2022). "The Role of 3D Printed Brain Models in Resident Education and Patient Communication." Journal of Medical Education, 97(8), 1123-1131.
Rodriguez, S. et al. (2021). "Cerebral Models and Their Impact on Reducing Surgical Risks in Complex Neurosurgical Cases." Neurosurgical Review, 44(2), 789-798.
Thompson, R. & Nakaji, P. (2023). "Revolutionizing Neurosurgical Planning: A Comprehensive Review of Cerebral Modeling Techniques." Neurosurgical Clinics of North America, 34(1), 1-14.