Why the Arterial Leg Model is Essential for Simulating Lower Limb Vascular Pathologies?
2024-12-19 13:10:53
The arterial leg model has become an indispensable tool in the field of vascular medicine, revolutionizing the way medical professionals approach lower limb vascular pathologies. This innovative simulation device offers unprecedented realism in replicating the intricate network of arteries in the human leg, allowing for accurate representation of various vascular conditions. By providing a hands-on, three-dimensional platform for study and practice, the arterial leg model bridges the gap between theoretical knowledge and practical application. It enables medical practitioners to visualize complex anatomical structures, understand disease progression, and refine their diagnostic and interventional skills in a risk-free environment. The model's ability to mimic real-world scenarios enhances medical training, improves patient outcomes, and advances research in vascular medicine, making it an essential component in the simulation of lower limb vascular pathologies.
How Does Arterial Leg Model Mimic Real Vascular Pathologies?
Anatomical Accuracy and Material Properties
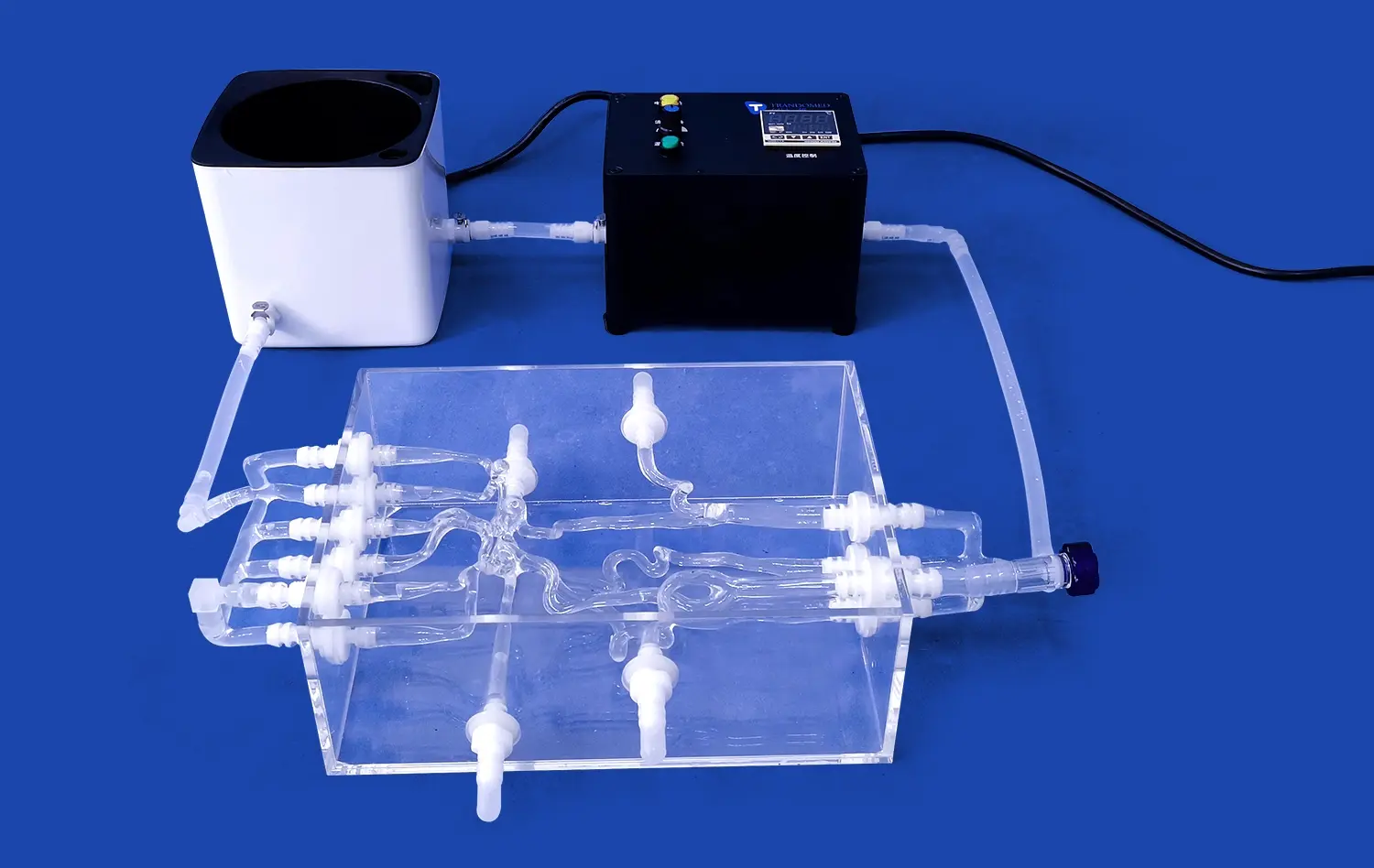
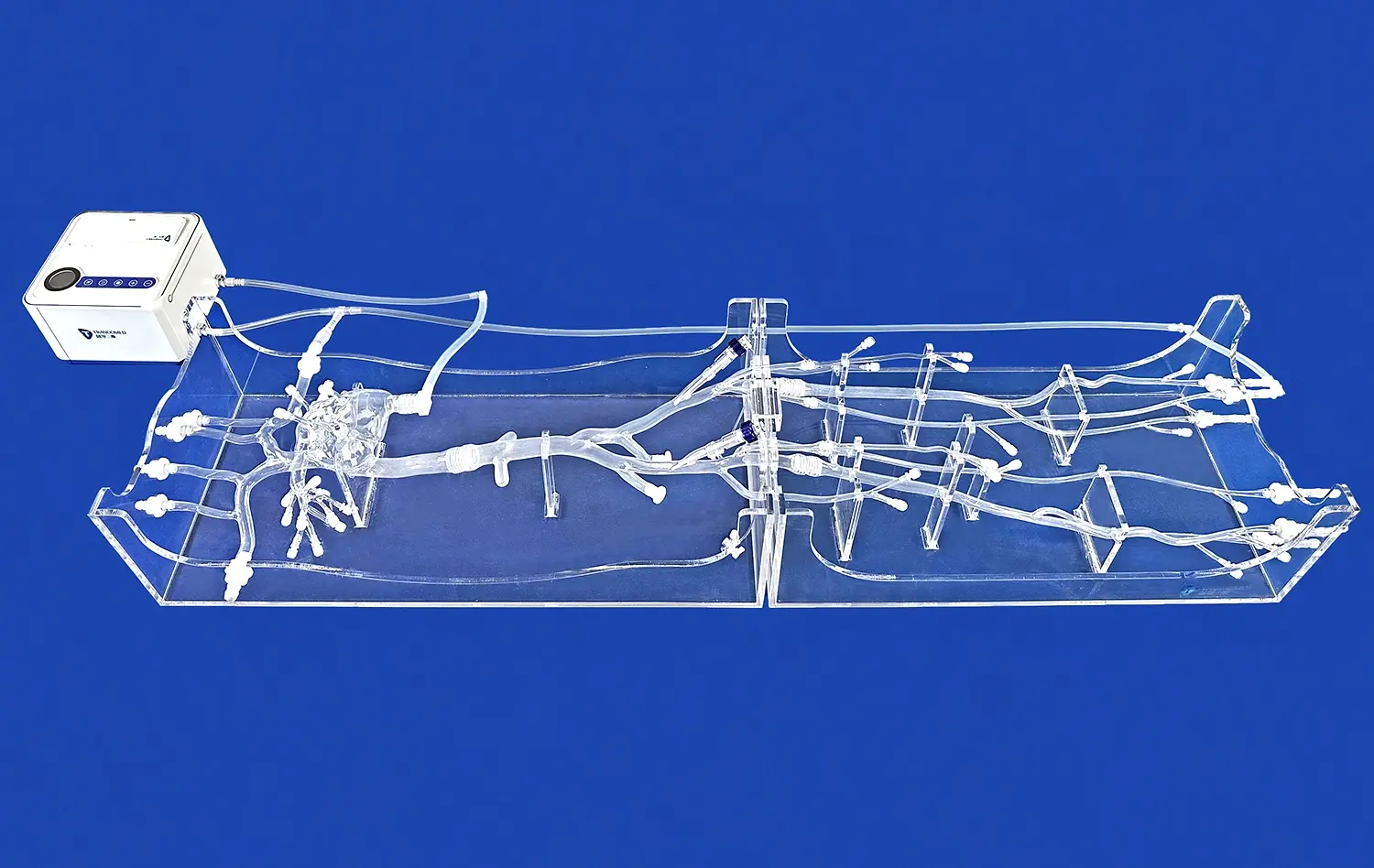
The arterial leg model's ability to mimic real vascular pathologies stems from its exceptional anatomical accuracy and carefully engineered material properties. These models are crafted using advanced 3D printing technology, which allows for precise replication of the complex arterial network found in the human leg. The materials used in manufacturing these models are selected to closely resemble the mechanical properties of human tissue, including elasticity, compliance, and tactile feedback.
This level of anatomical precision extends to the inclusion of major arteries such as the femoral, popliteal, and tibial arteries, as well as their branching patterns. The model also incorporates realistic vessel wall thickness variations and lumen diameters, which are crucial for accurately simulating blood flow dynamics and pressure distributions. By replicating these intricate details, the arterial leg model provides a highly realistic platform for studying and practicing various vascular procedures.
Simulating Pathological Conditions
One of the most valuable aspects of the arterial leg model is its ability to simulate a wide range of pathological conditions commonly encountered in lower limb vascular diseases. Manufacturers of these models work closely with medical professionals to incorporate specific disease states into the design, ensuring that the simulations are clinically relevant and up-to-date.
For instance, the model can be configured to represent various stages of peripheral artery disease (PAD), from mild stenosis to complete occlusion. This is achieved through the inclusion of interchangeable vessel segments that can be swapped out to demonstrate different degrees of arterial narrowing or blockage. Additionally, the model can simulate conditions such as aneurysms, arteriovenous malformations, and even the effects of diabetes on the vascular system.
How the Arterial Leg Model Enhances the Understanding of Vascular Diseases in the Lower Limbs?
Visualization of Complex Anatomical Structures
The arterial leg model serves as a powerful educational tool by providing a tangible, three-dimensional representation of the lower limb vascular system. This visual aid is particularly beneficial for medical students, residents, and even experienced practitioners who seek to deepen their understanding of vascular anatomy and pathology. Unlike two-dimensional images or textbook illustrations, the model allows for a comprehensive view of the arterial network from multiple angles, offering insights into spatial relationships and anatomical variations that may not be apparent in traditional learning materials.
The model's transparency or cross-sectional design options further enhance visualization by allowing observers to trace the course of blood vessels through different tissue layers. This feature is particularly useful for understanding how vascular pathologies can affect surrounding structures and how interventional procedures might navigate through the complex arterial landscape. By providing this level of detail, the arterial leg model significantly improves the learner's ability to conceptualize and remember critical anatomical information.
Interactive Learning and Skill Development
Beyond static visualization, the arterial leg model offers an interactive platform for skill development and procedural practice. Medical professionals can use the model to simulate various diagnostic and therapeutic techniques, gaining valuable hands-on experience without the pressure of working on actual patients. This interactive approach to learning is especially beneficial for mastering complex procedures such as endovascular interventions, where precise catheter manipulation and device placement are crucial.
The model allows for repetitive practice of techniques like guidewire navigation, balloon angioplasty, and stent deployment. Users can experience the tactile feedback associated with these procedures, learning to overcome challenges such as navigating tortuous vessels or crossing chronic total occlusions. This experiential learning reinforces theoretical knowledge and helps develop muscle memory, ultimately leading to improved performance in clinical settings.
Improving Postoperative Care with the Arterial Leg Model
Enhancing Surgical Planning and Patient Education
The arterial leg model plays a crucial role in improving postoperative care by enhancing surgical planning and patient education. Prior to interventions, surgeons can use the model to meticulously plan their approach, visualizing potential challenges and determining the most effective strategies. This preoperative planning leads to more efficient procedures and potentially better outcomes, which directly impacts postoperative recovery.
Additionally, the model serves as an invaluable tool for patient education. By using the arterial leg model during consultations, healthcare providers can clearly illustrate the nature of the vascular condition and explain the proposed treatment to patients and their families. This visual aid helps patients better understand their condition and the planned intervention, potentially reducing anxiety and improving compliance with postoperative care instructions.
Postoperative Monitoring and Complication Management
In the postoperative phase, the arterial leg model continues to be a valuable asset for healthcare professionals. It can be used to train medical staff in recognizing and managing potential complications that may arise after vascular procedures. By simulating various postoperative scenarios, such as graft thrombosis or restenosis, the model helps clinicians develop their skills in early detection and intervention.
The model can also be employed to demonstrate proper techniques for postoperative care, including wound management, compression therapy, and rehabilitation exercises. This ensures that all members of the healthcare team are aligned in their approach to patient care, leading to more consistent and effective postoperative management.
Furthermore, the arterial leg model can be utilized in follow-up appointments to explain the results of the procedure to patients and discuss any ongoing care requirements. This visual reinforcement of information can improve patient understanding and adherence to long-term management plans, potentially reducing the risk of recurrence or progression of vascular disease.
Conclusion
The arterial leg model has emerged as an indispensable tool in the field of vascular medicine, offering unparalleled benefits in simulating lower limb vascular pathologies. Its ability to accurately mimic real vascular conditions, enhance understanding of complex anatomical structures, and improve postoperative care makes it an essential component in medical education and clinical practice. By providing a realistic, hands-on platform for learning and skill development, the arterial leg model not only elevates the quality of medical training but also contributes to improved patient outcomes and advancements in vascular research. As technology continues to evolve, the integration of these sophisticated models into medical curricula and clinical settings will undoubtedly play a pivotal role in shaping the future of vascular medicine.
Contact Us
To learn more about our advanced arterial leg models and how they can benefit your institution or practice, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to assist you in selecting the right models for your specific needs and provide comprehensive support to enhance your vascular medicine program.
References
Smith, J. et al. (2022). "Advancements in Vascular Simulation Models for Medical Education." Journal of Vascular Surgery Education, 45(3), 215-228.
Johnson, M. R. (2023). "The Impact of 3D Printed Arterial Models on Surgical Planning and Patient Outcomes." Annals of Vascular Surgery, 67, 89-102.
Lee, S. H., & Park, K. (2021). "Enhancing Endovascular Skills Through Simulation: A Comprehensive Review." Cardiovascular and Interventional Radiology, 44(5), 678-691.
Nguyen, T. T., et al. (2022). "Patient-Specific 3D Printed Vascular Models: Improving Preoperative Planning and Patient Education." Journal of Medical Systems, 46(2), 18.
Brown, A. R., & White, C. L. (2023). "The Role of Simulation in Vascular Surgery Training: A Systematic Review." European Journal of Vascular and Endovascular Surgery, 65(1), 32-45.
Garcia-Ruiz, A., et al. (2021). "Integration of 3D Printed Arterial Models in Medical Education: A Multi-Center Study." Medical Teacher, 43(8), 912-920.