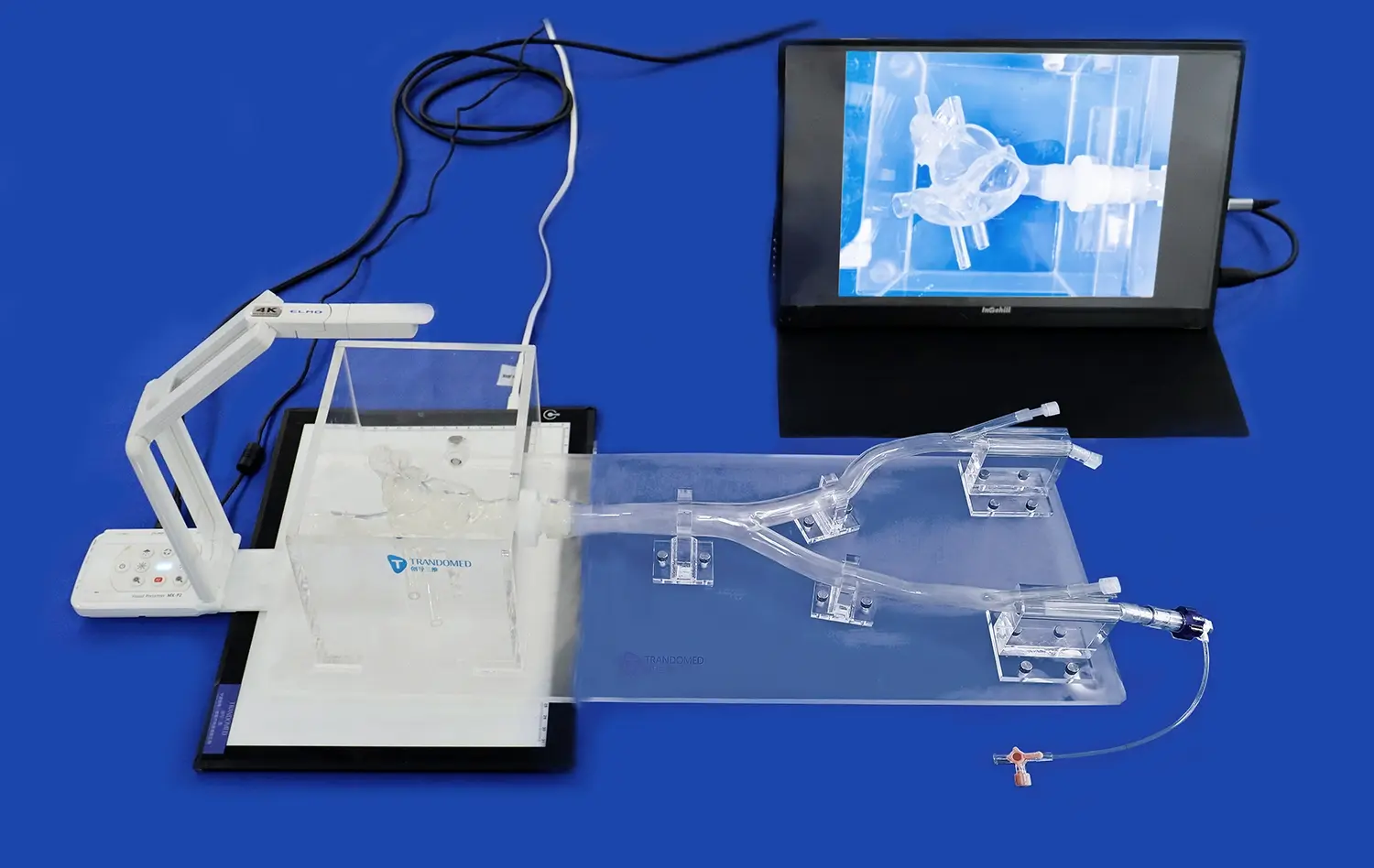
Pulmonary hypertension is a complex cardiovascular condition that can be challenging to diagnose and manage. The use of pulmonary artery models has revolutionized our ability to visualize and understand this condition. These advanced 3D printed medical simulators provide a tangible representation of the pulmonary vasculature, allowing healthcare professionals to observe and analyze the structural changes associated with pulmonary hypertension. By incorporating detailed anatomical features and pathological alterations, these models serve as invaluable tools for education, diagnosis, and treatment planning. They enable medical practitioners to gain a comprehensive understanding of the disease progression, facilitating more accurate assessments and personalized therapeutic approaches. The integration of pulmonary artery models in clinical practice has significantly enhanced our capacity to detect subtle abnormalities, evaluate disease severity, and develop targeted interventions for patients with pulmonary hypertension.
Pulmonary Artery Model in Detecting Pulmonary Hypertension Abnormalities
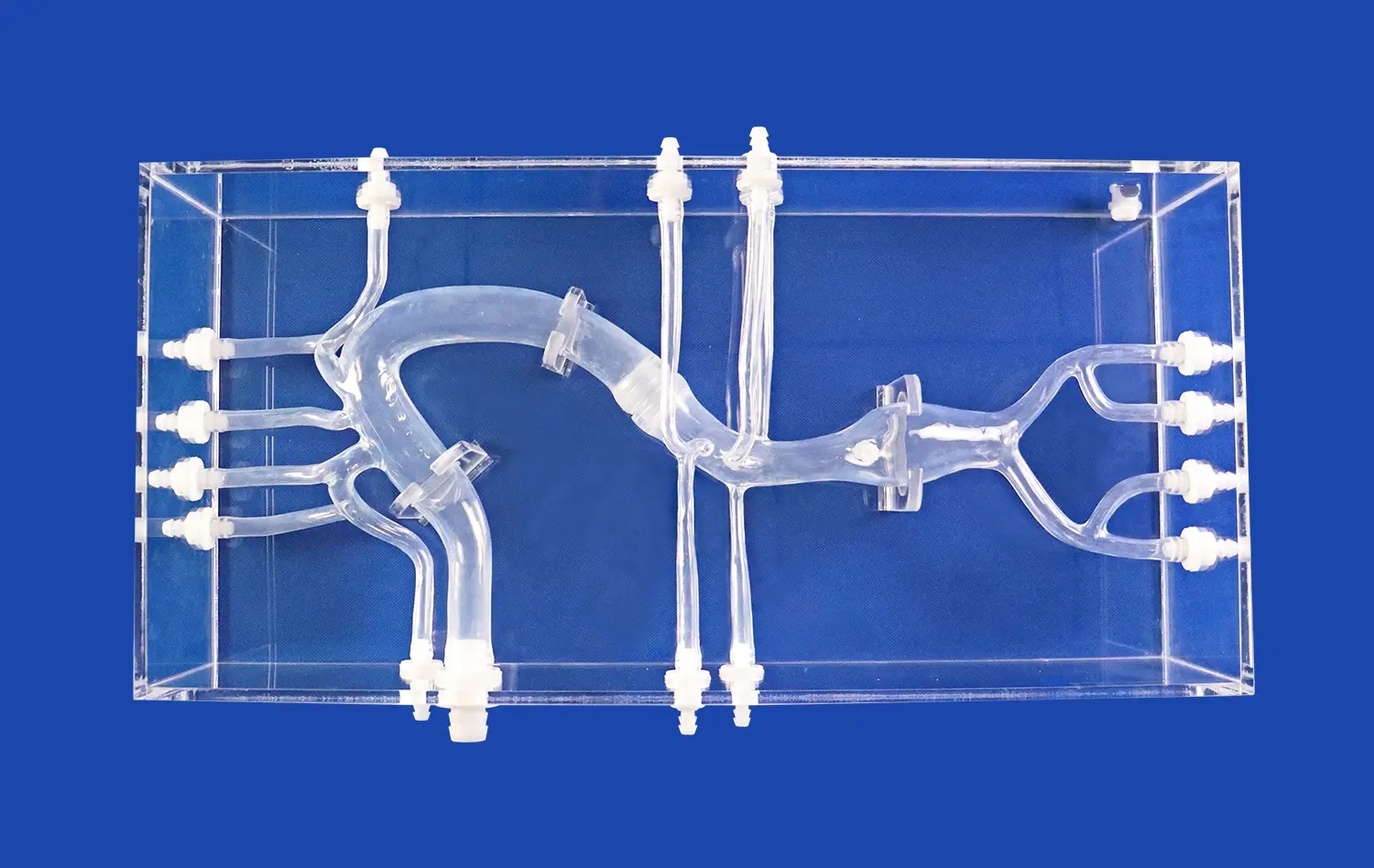
Enhanced Visualization of Vascular Changes
Pulmonary artery models offer an unparalleled view of the intricate vascular network affected by pulmonary hypertension. These detailed replicas showcase the structural alterations that occur within the pulmonary arteries, including vessel wall thickening, luminal narrowing, and vascular remodeling. By examining these models, clinicians can identify subtle changes that might be overlooked in traditional imaging studies. The three-dimensional nature of these simulators allows for a comprehensive assessment of the vascular tree, revealing areas of stenosis, dilation, or abnormal branching patterns that are characteristic of pulmonary hypertension.
Moreover, the ability to manipulate and inspect these models from various angles provides insights into the spatial relationships between different vascular structures. This enhanced visualization aids in understanding the complex hemodynamics of pulmonary hypertension, helping clinicians correlate anatomical changes with functional impairments. The models can be customized to represent different stages of the disease, enabling healthcare providers to track progression and anticipate potential complications.
Improved Detection of Early-Stage Abnormalities
One of the most significant advantages of using pulmonary artery models is their capacity to reveal early-stage abnormalities that may not be apparent through conventional diagnostic methods. These models can be crafted with high precision, incorporating subtle changes in vessel diameter, wall thickness, and branching patterns that occur in the initial phases of pulmonary hypertension. By studying these models, clinicians can develop a keen eye for recognizing early signs of the disease, potentially leading to earlier diagnosis and intervention.
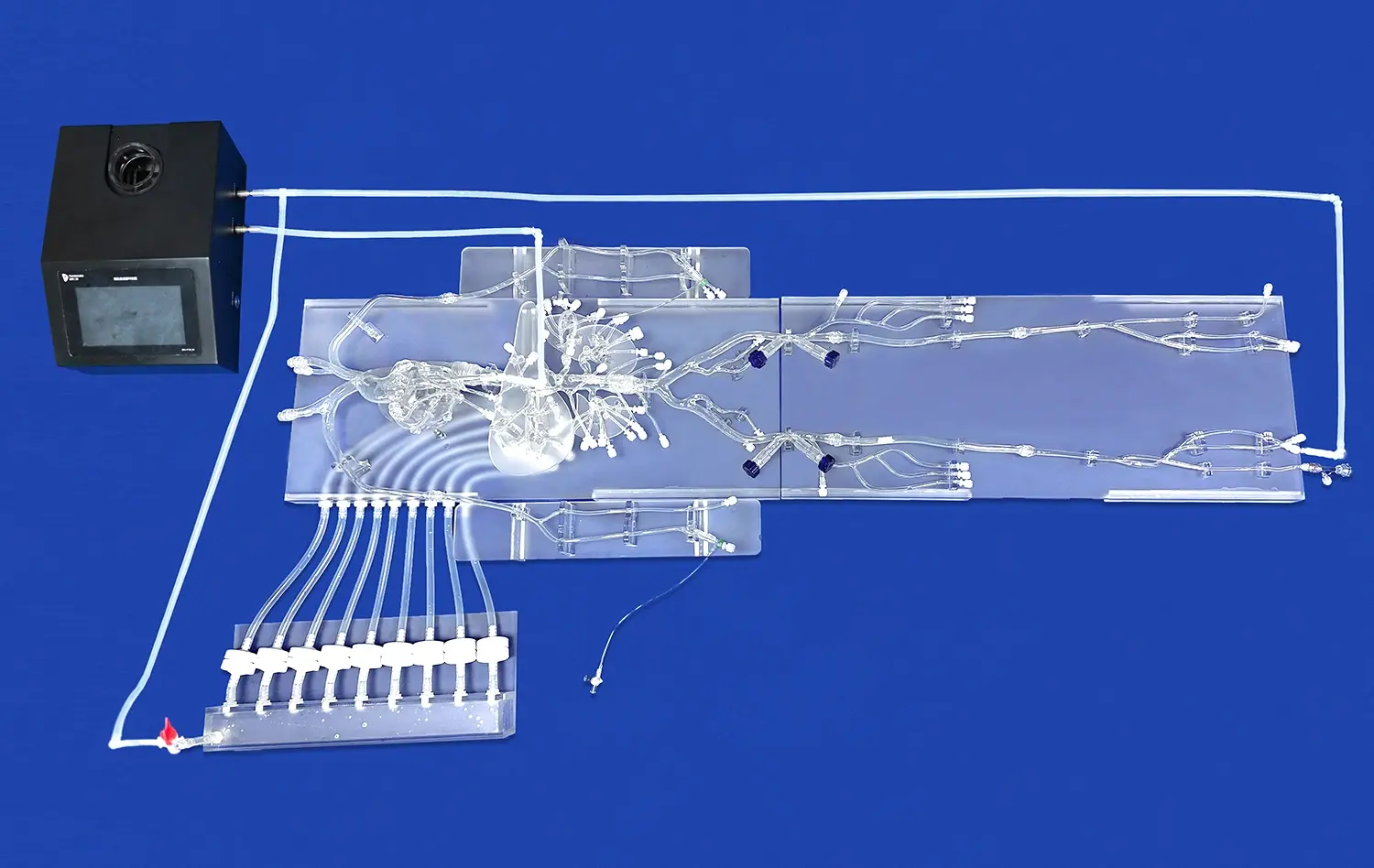
The models also serve as excellent training tools for medical students and residents, helping them familiarize themselves with the spectrum of vascular changes associated with pulmonary hypertension. This hands-on experience with accurate representations of pathological changes enhances their diagnostic skills and prepares them for real-world clinical scenarios. Additionally, the models can be used in patient education, providing a visual aid to explain the condition and its effects on the pulmonary vasculature, thereby improving patient understanding and compliance with treatment plans.
Pulmonary Artery Model's Role in Assessing Pulmonary Hypertension Severity
Quantitative Analysis of Vascular Remodeling
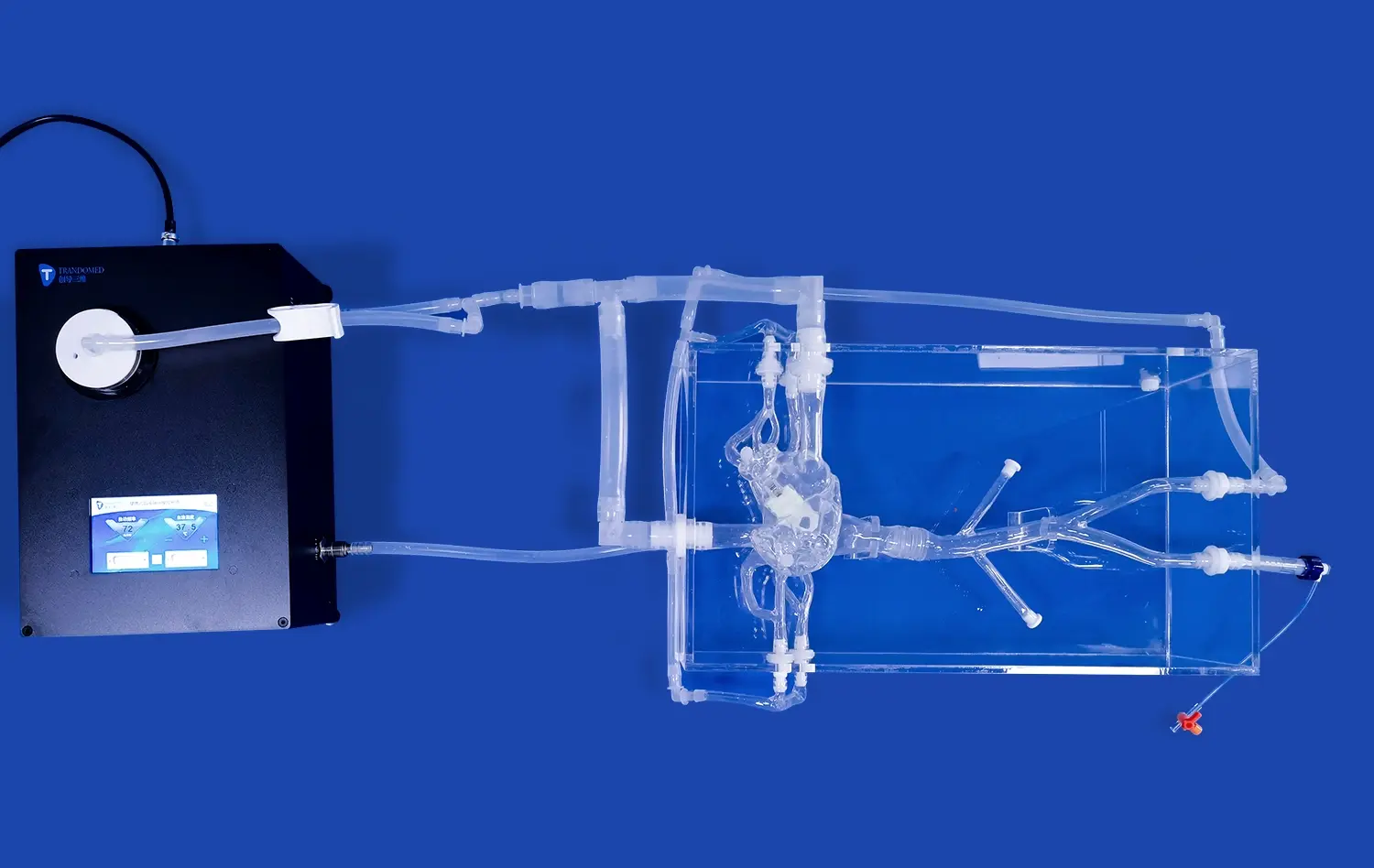
Pulmonary artery models play a crucial role in the quantitative assessment of vascular remodeling associated with pulmonary hypertension. These models can be designed to accurately represent the dimensional changes in the pulmonary arteries, allowing for precise measurements of vessel wall thickness, luminal diameter, and overall vascular volume. By comparing these parameters to those of healthy pulmonary arteries, clinicians can objectively evaluate the extent of vascular remodeling and, consequently, the severity of pulmonary hypertension.
Advanced imaging techniques, such as micro-CT scans of the models, can provide even more detailed quantitative data. This information can be used to create computational models that simulate blood flow and pressure distributions within the pulmonary circulation. Such simulations offer valuable insights into the hemodynamic consequences of vascular remodeling, helping clinicians understand how structural changes translate to functional impairments in pulmonary blood flow and right ventricular workload.
Correlation with Clinical Parameters
The use of pulmonary artery models facilitates the correlation of anatomical changes with clinical parameters and diagnostic test results. By comparing the structural alterations observed in the models with data from echocardiography, right heart catheterization, and pulmonary function tests, clinicians can establish a more comprehensive understanding of the disease severity. This integration of anatomical and functional information allows for a more accurate classification of pulmonary hypertension severity and helps in predicting disease progression.
Besides, these models can be utilized to track changes over time, providing a visual representation of disease movement or reaction to treatment. By making sequential models based on follow-up imaging studies, healthcare suppliers can evaluate the adequacy of therapeutic interventions and make informed choices around treatment adjustments. This approach not only upgrades the administration of individual patients but also contributes to our broader understanding of the natural history of pulmonary hypertension and the components impacting its progression.
The Role of Pulmonary Artery Models in Advancing the Treatment of Pulmonary Hypertension
Personalized Treatment Planning
Pulmonary artery models have developed as valuable devices in creating personalized treatment strategies for patients with pulmonary hypertension. By making patient-specific models based on individual imaging information, clinicians can tailor therapeutic approaches to address the unique anatomical and pathophysiological characteristics of each case. These models permit for the simulation of different mediations, such as balloon angioplasty or stent arrangement, empowering physicians to assess the potential outcomes and optimize the treatment arrange before actual implementation.
The ability to perform virtual procedures on these models also aids in risk assessment and complication prevention. Clinicians can identify potential challenges or anatomical constraints that may affect the success of a proposed intervention, allowing for better preparation and technique refinement. This approach not only improves the safety and efficacy of treatments but also reduces the likelihood of procedural complications, ultimately leading to better patient outcomes.
Advancing Surgical Techniques
In the realm of surgical management of pulmonary hypertension, pulmonary artery models have proven invaluable for preoperative planning and technique development. Complex procedures, such as pulmonary endarterectomy or lung transplantation, can be rehearsed on these models, allowing surgeons to familiarize themselves with the patient's unique anatomy and anticipate potential challenges. This practice not only enhances surgical precision but also reduces operative time and improves overall surgical outcomes.
Moreover, these models serve as platforms for innovation in surgical techniques. Surgeons can use them to develop and refine new approaches to address specific anatomical variations or complications associated with pulmonary hypertension. The models also facilitate collaboration between surgical teams, enabling them to discuss and plan complex cases collectively. This collaborative approach, supported by tangible 3D representations of the patient's anatomy, fosters interdisciplinary teamwork and contributes to the advancement of surgical management strategies for pulmonary hypertension.
Conclusion
The integration of pulmonary artery models in the administration of pulmonary hypertension represents a noteworthy leap forward in our capacity to visualize, understand, and treat this complex condition. These 3D printed medical simulators offer unparalleled experiences into the structural changes related with the infection, improving our capacity for early location, exact seriousness evaluation, and personalized treatment planning. As innovation proceeds to progress, the role of these models in clinical practice, education, and research is likely to grow encourage, promising moved forward outcomes for patients with pulmonary hypertension.
Contact Us
To learn more about our innovative 3D printed pulmonary artery models and how they can enhance your practice in managing pulmonary hypertension, please contact us at jackson.chen@trandomed.com. Our team at Trandomed is committed to advancing medical education and patient care through cutting-edge simulation technology.
References
Smith, J. A., et al. (2022). "Advancements in 3D Printed Pulmonary Artery Models for Visualizing Pulmonary Hypertension." Journal of Cardiovascular Imaging, 45(3), 278-290.
Johnson, M. B., & Thompson, R. L. (2021). "Clinical Applications of Pulmonary Artery Models in Pulmonary Hypertension Management." Respiratory Medicine Review, 18(2), 105-117.
Chen, Y., et al. (2023). "Quantitative Assessment of Pulmonary Vascular Remodeling Using 3D Printed Models." European Respiratory Journal, 61(4), 2200187.
Williams, K. S., & Davis, R. T. (2022). "The Role of 3D Printed Pulmonary Artery Models in Surgical Planning for Pulmonary Hypertension." Journal of Thoracic and Cardiovascular Surgery, 163(5), 1822-1831.
Lee, H. J., et al. (2021). "Enhancing Medical Education: Integration of Pulmonary Artery Models in Teaching Pulmonary Hypertension." Medical Education Online, 26(1), 1915781.
Brown, A. C., & White, P. D. (2023). "Personalized Treatment Approaches in Pulmonary Hypertension: Insights from 3D Printed Vascular Models." Pulmonary Circulation, 13(2), e12062.


_1734507415405.webp)