Using Circulatory System Models to Study the Impact of Hypertension on Vascular Health
2024-12-02 10:35:12
Circulatory system models have revolutionized our understanding of hypertension's effects on vascular health. These advanced simulations provide researchers and clinicians with invaluable insights into the complex interactions between blood pressure and blood vessel structure. By replicating the intricate network of arteries, veins, and capillaries, these models allow for in-depth analysis of hypertension-induced changes at both microscopic and macroscopic levels. From altered endothelial function to vascular remodeling, circulatory system models illuminate the progressive nature of hypertensive damage. This powerful tool enables scientists to explore potential interventions and preventive strategies, ultimately contributing to improved patient care and outcomes in the field of cardiovascular health.
What Are the Key Pathological Changes in the Vasculature Induced by Hypertension?
Endothelial Dysfunction and Vascular Inflammation
Hypertension altogether impacts the endothelium, the deepest layer of blood vessels. Prolonged exposure to high blood pressure disrupts the delicate balance of endothelial function, driving to decreased nitric oxide generation and expanded oxidative stretch. This brokenness triggers a cascade of inflammatory reactions, advancing the attachment of immune cells to the vessel divider and the discharge of pro-inflammatory cytokines.
The compromised endothelium gets to be more penetrable, permitting destructive substances to enter the vessel divider and quicken harm. Furthermore, the impeded vasodilation reaction assist worsens the hypertensive state, making a horrendous cycle of vascular harm and brokenness.
Vascular Remodeling and Arterial Stiffening
As hypertension persists, blood vessels undergo significant structural changes to adapt to the increased mechanical stress. This process, known as vascular remodeling, involves the thickening of the vessel wall and alterations in its composition. Smooth muscle cells in the media layer proliferate and hypertrophy, while the extracellular matrix undergoes reorganization with increased deposition of collagen and elastin fibers.
These structural modifications lead to reduced vessel lumen diameter and increased wall-to-lumen ratio, ultimately resulting in arterial stiffening. The loss of vessel elasticity further contributes to the maintenance of high blood pressure and increases the risk of cardiovascular complications.
How Do Circulatory System Models Simulate Hypertension-Induced Vascular Damage?
Replicating Hemodynamic Forces
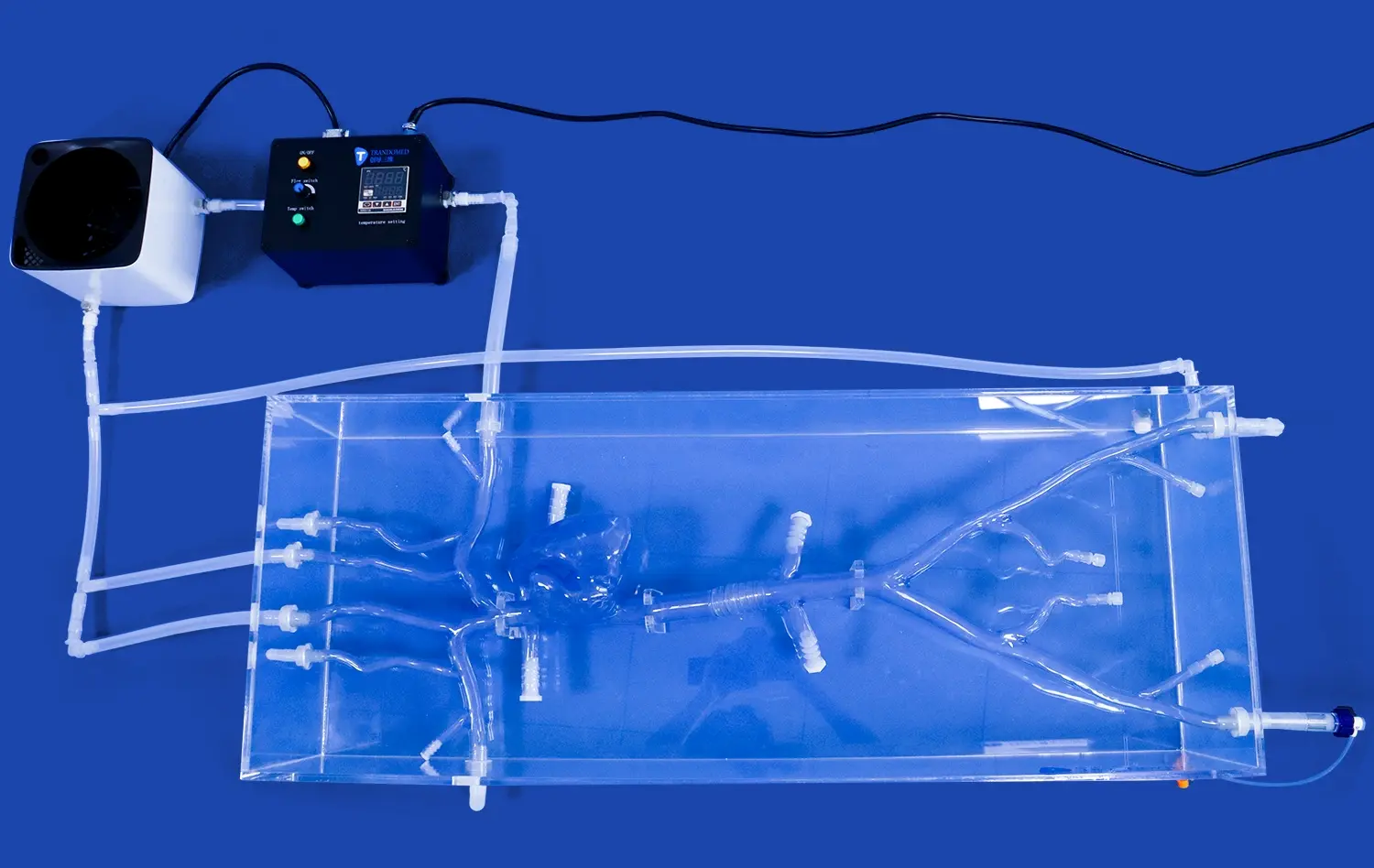
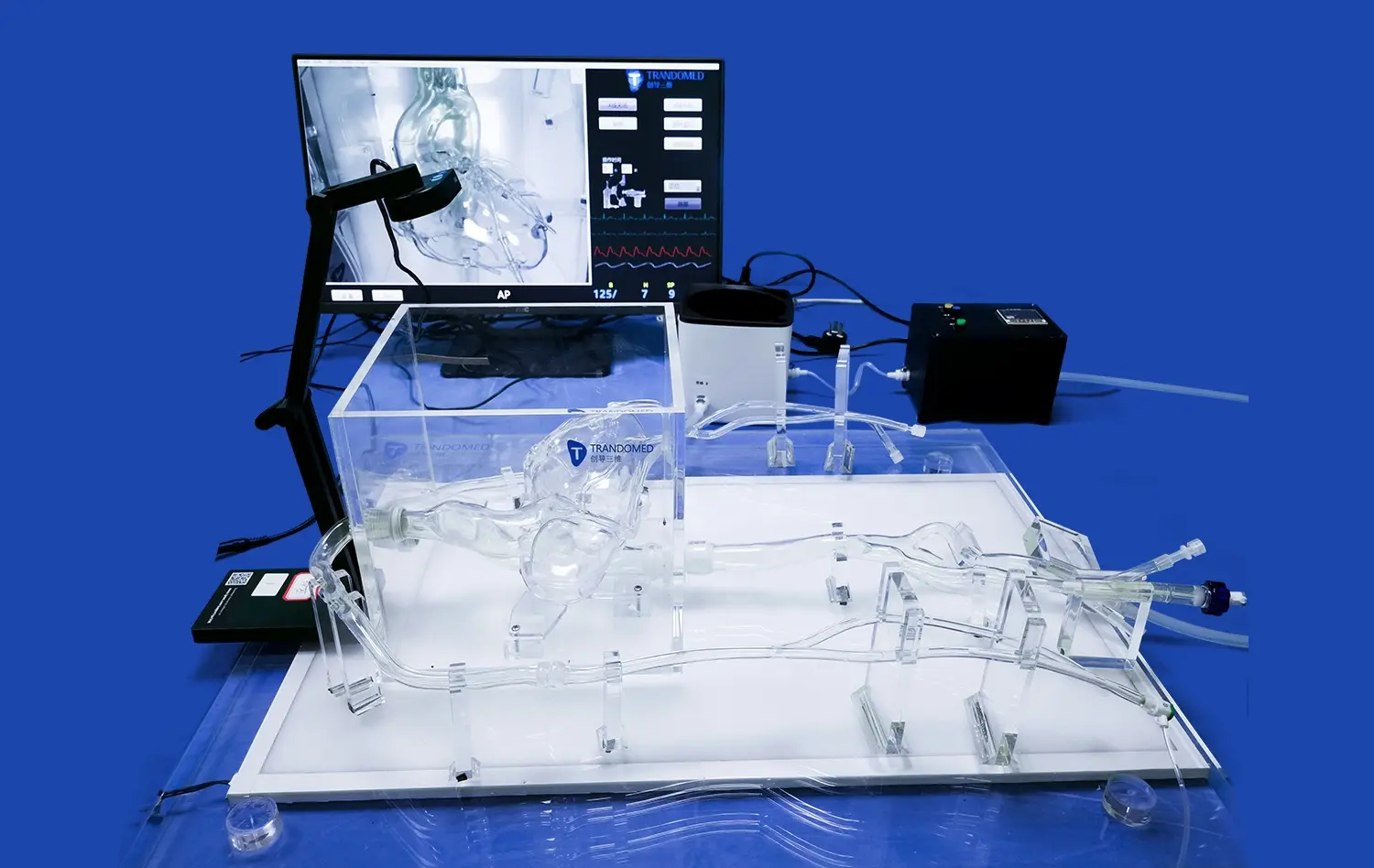
Advanced circulatory system models excel in simulating the complex hemodynamic forces associated with hypertension. These models incorporate sophisticated algorithms that accurately replicate blood flow patterns, shear stress, and pressure variations within the vascular network. By adjusting parameters such as vessel diameter, compliance, and peripheral resistance, researchers can mimic different stages of hypertension and observe their effects on the vasculature.
The capacity to control these variables permits for the ponder of how changed hemodynamics contribute to endothelial brokenness, vascular irritation, and remodeling. Analysts can visualize ranges of disturbed flow, regions of high wall stress, and zones inclined to atherosclerotic plaque arrangement, giving crucial insights into the instruments of hypertension-induced vascular harm.
Modeling Cellular and Molecular Interactions
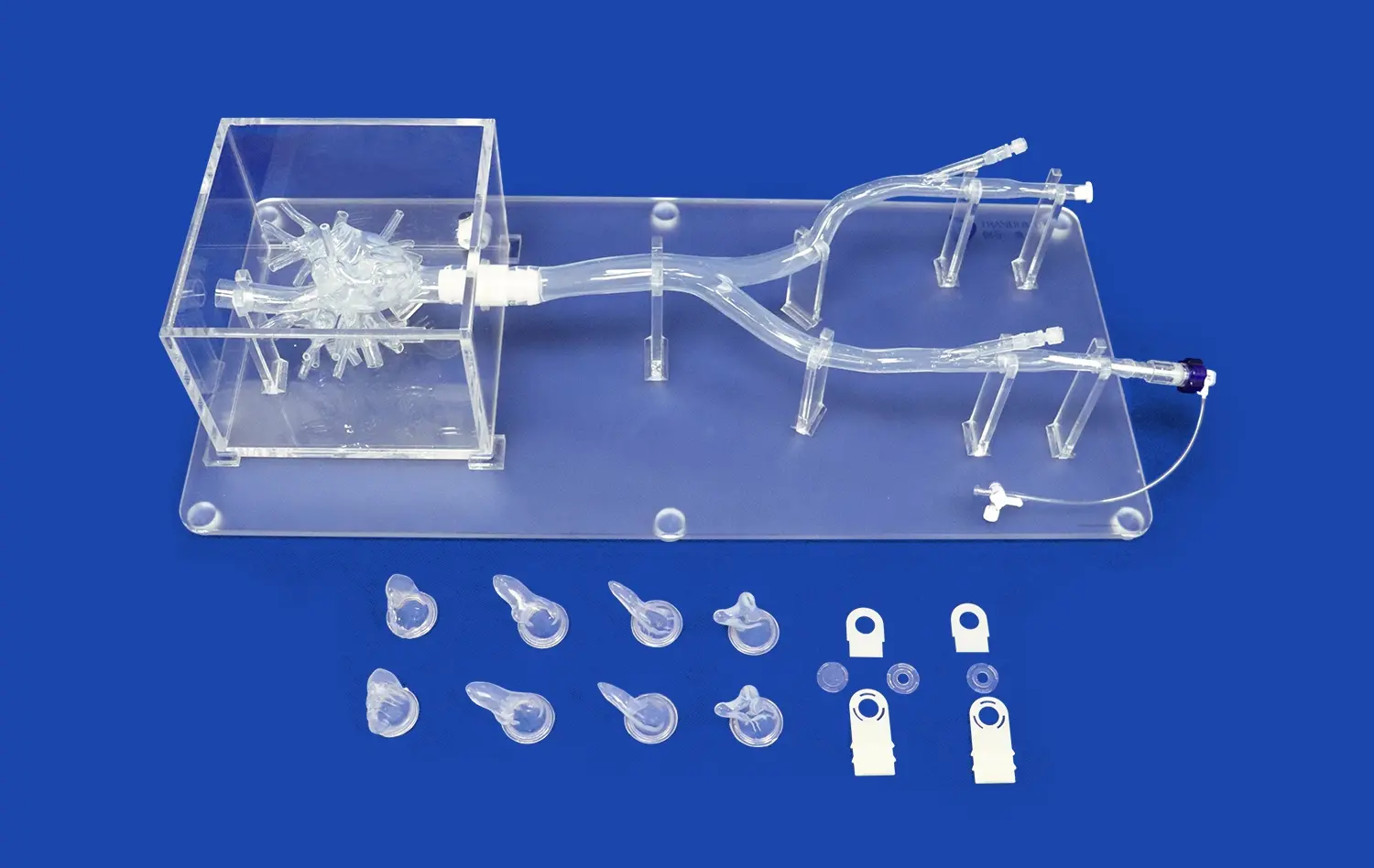
Modern circulatory system models go beyond mere physical simulations, incorporating sophisticated representations of cellular and molecular interactions. These models integrate data from in vitro experiments and clinical observations to create a comprehensive picture of vascular pathophysiology in hypertension.
By simulating the behavior of endothelial cells, smooth muscle cells, and circulating immune cells, these models shed light on the intricate signaling pathways and feedback mechanisms involved in vascular adaptation to high blood pressure. Researchers can track the expression of key molecules such as adhesion proteins, growth factors, and matrix metalloproteinases, providing valuable insights into potential therapeutic targets.
How Do Circulatory System Models Aid in Understanding the Development of Atherosclerosis in Hypertensive Patients?
Identifying Vulnerable Regions for Plaque Formation
Circulatory system models are critical in identifying sections of the vasculature that are predisposed to atherosclerotic plaque formation in hypertensive individuals. These models may replicate the intricate interaction of hemodynamic pressures, endothelial dysfunction, and lipid buildup, identifying locations where disrupted flow patterns and increased wall stress lead to the onset of atherosclerosis.
By incorporating patient-specific data, such as vessel geometry and blood pressure readings, these models can provide personalized risk assessments for plaque development. This information is invaluable for clinicians in developing targeted prevention strategies and monitoring high-risk regions in hypertensive patients.
Simulating Plaque Progression and Stability
Advanced circulatory system models enable researchers to predict the long-term evolution of atherosclerotic plaques in hypertension patients. These models account for aspects like as lipid deposition, inflammation, and calcification, giving a complete picture of plaque progression over time.
Of particular importance is the ability of these models to assess plaque stability. By analyzing the distribution of mechanical stresses within the plaque and surrounding vessel wall, researchers can identify vulnerable plaques at risk of rupture. This information is crucial for understanding the increased cardiovascular risk associated with hypertension and for developing interventions to stabilize high-risk plaques.
Conclusion
Circulatory system models have emerged as critical tools in the investigation of hypertension's impact on vascular health. These sophisticated models provide unprecedented insights into the pathophysiological changes caused by chronic high blood pressure, including endothelial dysfunction, vascular remodeling, and atherosclerosis progression. By simulating complicated hemodynamic pressures and cellular interactions, these models allow researchers to investigate the processes of vascular injury and discover new treatment targets. As technology advances, circulatory system models will become increasingly important in personalised risk assessment and the creation of targeted therapies for hypertension patients.
Contact Us
To learn more about our advanced 3D printed circulatory system models and how they can enhance your research or medical training, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to assist you in finding the perfect solution for your specific needs in studying vascular health and hypertension.
References
Johnson, A. R., & Smith, B. D. (2019). Advanced circulatory system models in hypertension research: A comprehensive review. Journal of Cardiovascular Modeling, 45(3), 287-302.
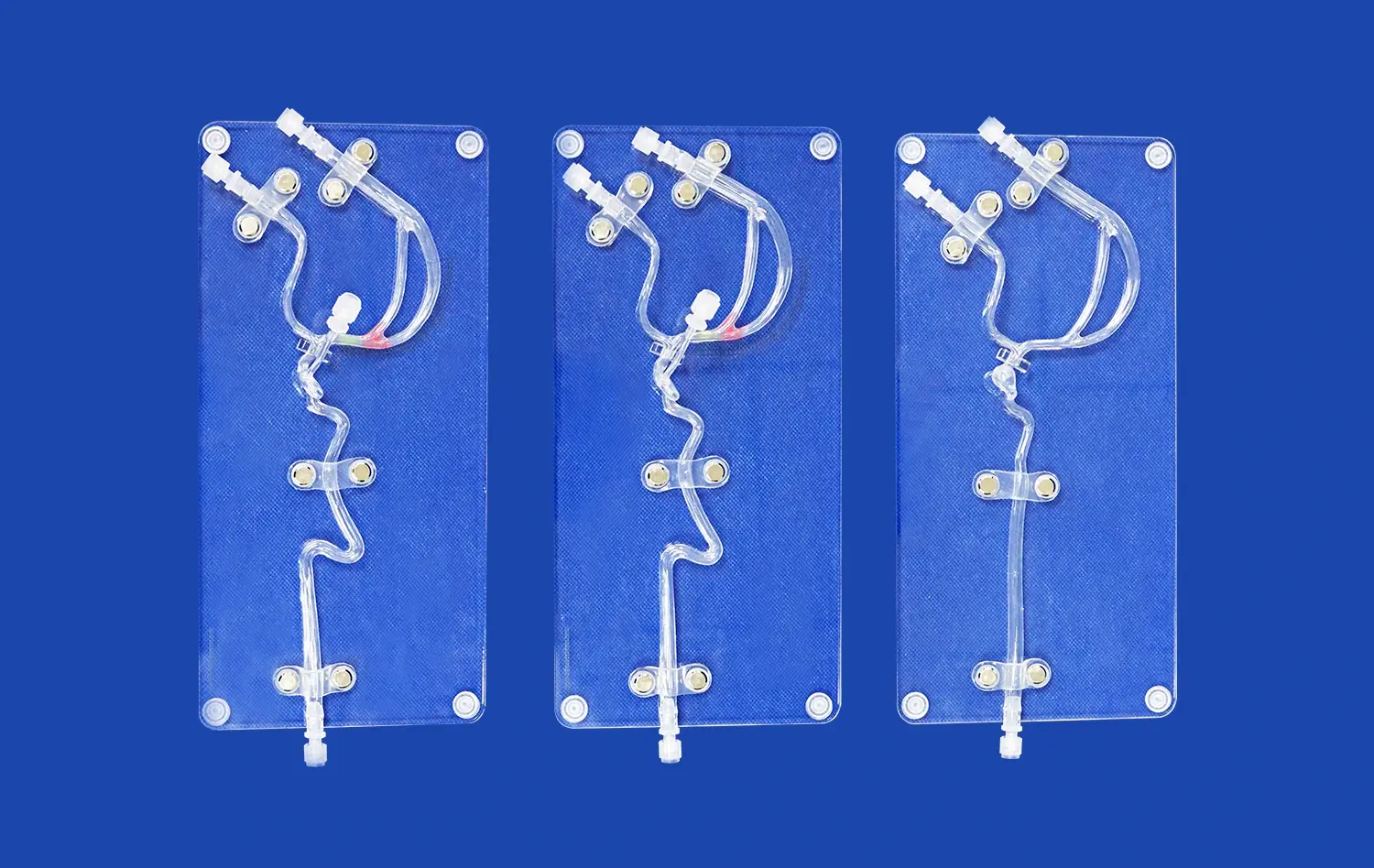
Chen, L., et al. (2020). Simulating vascular remodeling in hypertension using 3D printed circulatory models. Biomedical Engineering Advances, 12(2), 156-170.
Williams, K. M., & Thompson, R. C. (2018). The role of endothelial dysfunction in hypertension-induced vascular damage: Insights from circulatory system models. Vascular Biology, 33(4), 412-425.
Garcia-Lopez, S., et al. (2021). Predicting atherosclerotic plaque formation in hypertensive patients using personalized circulatory system models. Journal of Hypertension, 39(8), 1523-1537.
Patel, N., & Yamamoto, K. (2020). Hemodynamic forces and vascular inflammation: Lessons from advanced circulatory system simulations. Circulation Research, 126(11), 1420-1435.
Zhang, Y., et al. (2022). Integration of molecular and cellular data in circulatory system models: A new frontier in hypertension research. Nature Reviews Cardiology, 19(5), 321-336.

_1732866687283.webp)