Understanding the Importance of PCI Models in Simulating Real-World Coronary Interventions
2024-12-13 15:52:25
Percutaneous Coronary Intervention (PCI) models have revolutionized the way we approach coronary interventions, offering invaluable insights into complex cardiac procedures. These sophisticated simulations provide a safe, controlled environment for healthcare professionals to hone their skills and test innovative techniques. By replicating the intricate anatomy of coronary arteries and mimicking various pathological conditions, PCI models enable interventional cardiologists to practice and perfect their techniques without risking patient safety. This advanced technology not only enhances the quality of medical training but also accelerates the development and validation of new devices and treatment strategies, ultimately leading to improved patient outcomes in real-world scenarios.
What Are PCI Models and How Do They Simulate Real-World Coronary Interventions?
The Anatomy of PCI Models
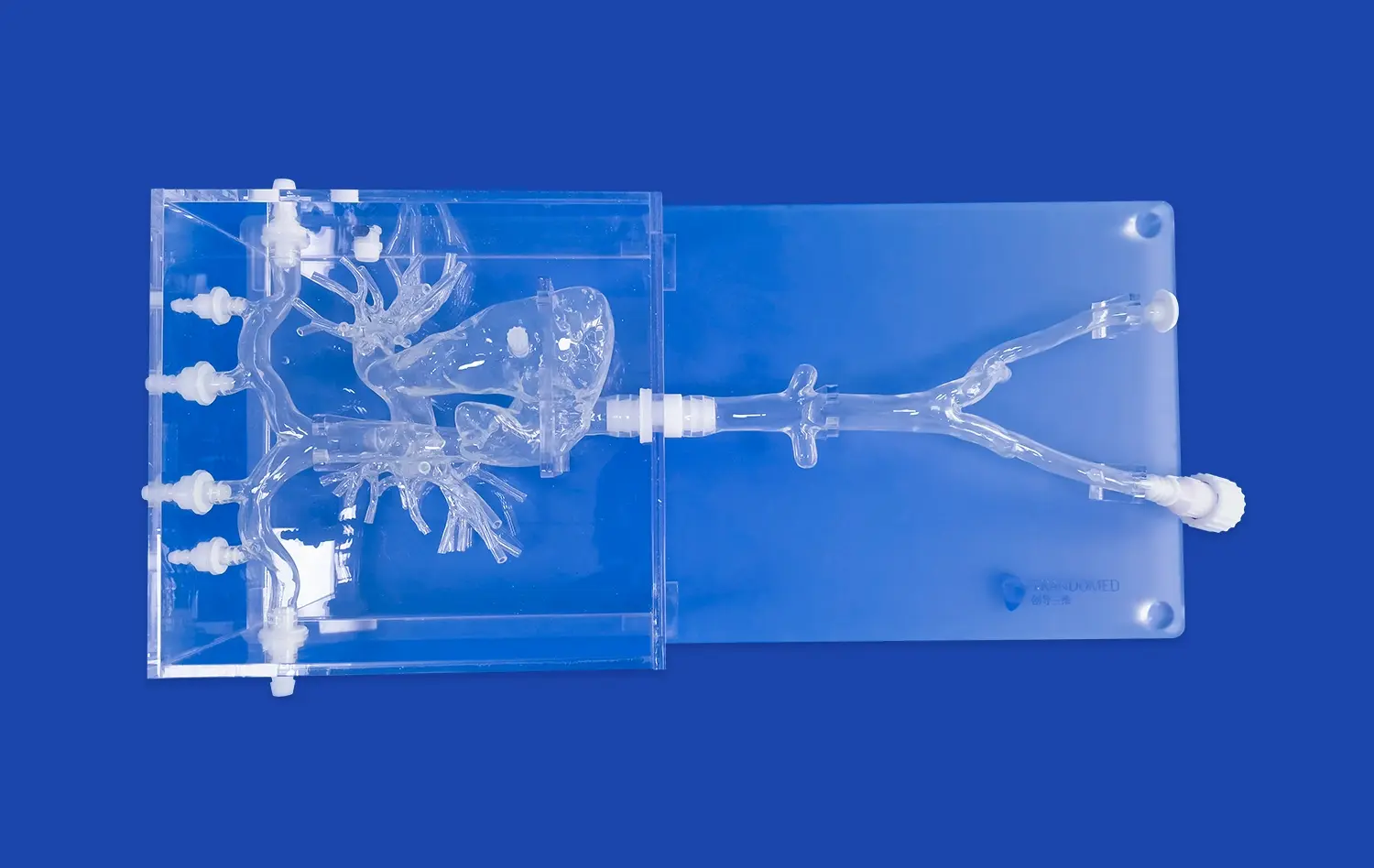
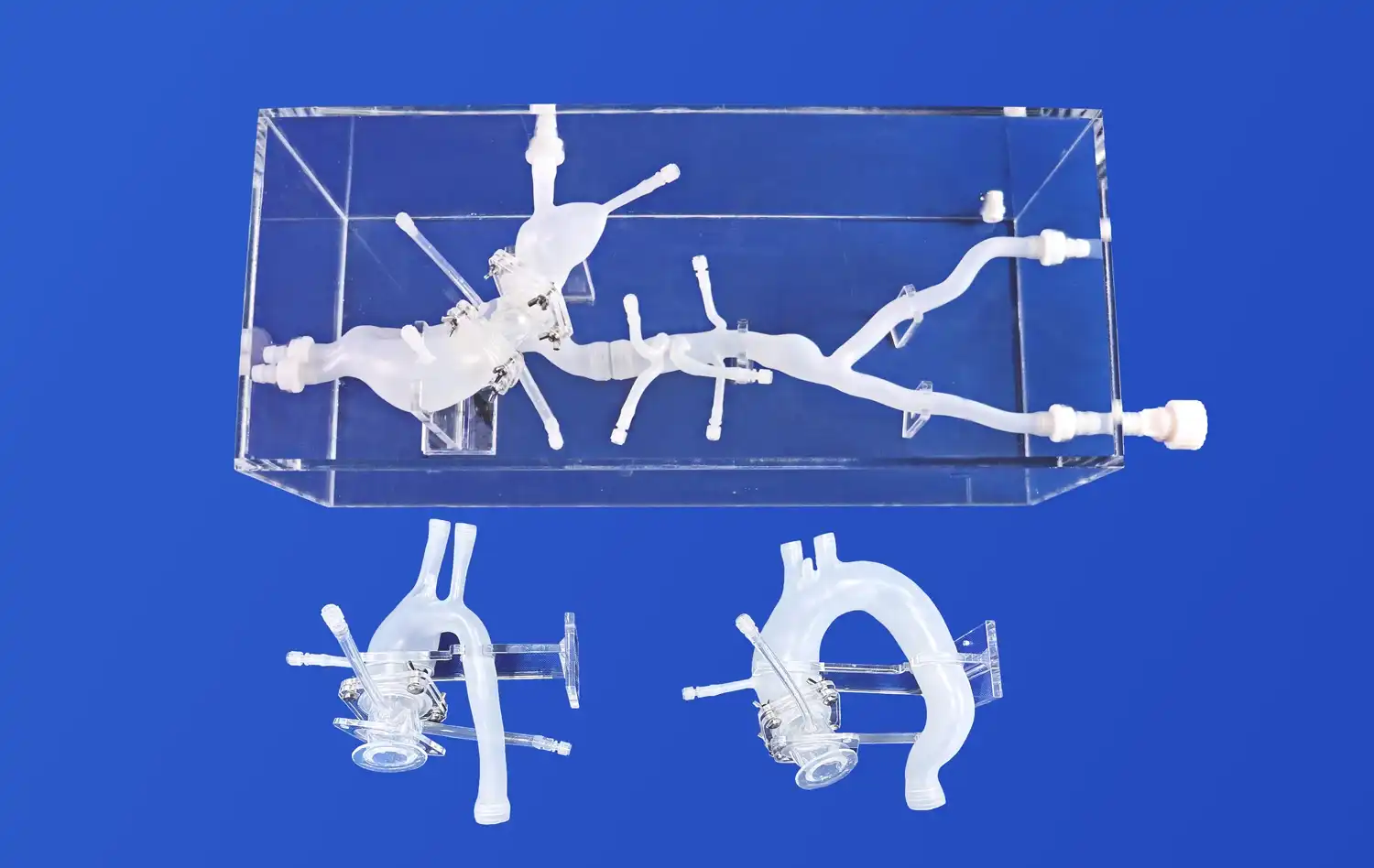
PCI models are meticulously designed replicas of the human coronary system, crafted to mimic the intricate network of arteries that supply blood to the heart. These models are typically created using advanced 3D printing technologies and high-quality silicone materials, ensuring a realistic look and feel. The anatomy includes the main coronary arteries - left anterior descending (LAD), left circumflex (LCX), and right coronary artery (RCA) - along with their branches and varying degrees of stenosis or blockages.
The models are designed to replicate various pathological conditions commonly encountered in clinical practice, such as calcified lesions, bifurcation lesions, and chronic total occlusions. This level of detail allows interventional cardiologists to practice navigating through complex anatomical structures and dealing with challenging scenarios they might face in real patients.
Simulating Real-World Interventions
PCI models go beyond static representations by incorporating dynamic elements that simulate the physiological conditions of the heart. These may include:
- Pulsatile flow systems that mimic blood flow through the coronary arteries
- Adjustable pressure gradients to simulate different hemodynamic conditions
- Radiopaque markers for fluoroscopic guidance during simulated procedures
- Replaceable stenotic segments to practice various intervention techniques
By integrating these features, PCI models create a highly realistic environment for practicing coronary interventions. Clinicians can perform a wide range of procedures, including balloon angioplasty, stent deployment, and complex techniques like bifurcation stenting or chronic total occlusion recanalization. The ability to repeat procedures, adjust variables, and receive immediate feedback makes these models invaluable tools for both training and research purposes.
Why Are PCI Models Crucial for Testing New Devices and Technologies in Coronary Interventions?
Accelerating Innovation in Interventional Cardiology
PCI models play a pivotal role in the development and validation of new interventional devices and technologies. They serve as a critical bridge between in vitro testing and clinical trials, offering a controlled environment to assess the performance, safety, and efficacy of novel tools and techniques. This accelerates the innovation process by:
- Allowing rapid prototyping and iterative design improvements
- Providing a platform for comparing new devices against existing standards
- Enabling the assessment of device performance under various anatomical and physiological conditions
- Facilitating the development of new intervention strategies and techniques
By using PCI models, researchers and device manufacturers can identify potential issues early in the development process, refine their designs, and optimize performance before proceeding to costly and time-consuming clinical trials. This not only streamlines the innovation pipeline but also enhances the safety and efficacy of new technologies before they reach patients.
Enhancing Training and Skill Development
PCI models are indispensable tools for training interventional cardiologists and improving their skills. These models offer several advantages over traditional training methods:
- Risk-free environment for practicing complex procedures
- Standardized scenarios for objective skill assessment
- Opportunity to practice rare or high-risk cases repeatedly
- Immediate feedback on performance and outcomes
By incorporating PCI models into training programs, healthcare institutions can ensure that their interventional cardiologists are well-prepared to handle a wide range of clinical scenarios. This leads to improved procedural outcomes, reduced complications, and enhanced patient safety in real-world interventions.
What Are the Future Trends in PCI Modeling and Its Potential Impact on Coronary Interventions?
Advancements in Model Fidelity and Functionality
The future of PCI model is poised for significant advancements that will further enhance its utility in both training and research. Some emerging trends include:
- Integration of artificial intelligence for more realistic tissue responses
- Incorporation of patient-specific data to create personalized models
- Development of hybrid models combining physical and virtual elements
- Enhanced tactile feedback systems for improved haptic realism
These advancements will lead to even more accurate simulations of coronary interventions, allowing for more precise training and testing of new devices and techniques. As model fidelity improves, the gap between simulation and real-world procedures will continue to narrow, further enhancing the value of PCI models in interventional cardiology.
Expanding Applications in Precision Medicine
The evolution of PCI models is expected to have a profound impact on the field of precision medicine in cardiology. Future applications may include:
- Pre-procedural planning using patient-specific 3D printed models
- Virtual trials to predict individual patient responses to different interventions
- Integration with computational fluid dynamics for optimized stent placement
- Development of tailored intervention strategies based on simulated outcomes
By leveraging advanced PCI models in combination with patient-specific data, interventional cardiologists will be better equipped to make informed decisions and customize treatments for individual patients. This approach has the potential to significantly improve procedural success rates, reduce complications, and enhance overall patient outcomes in coronary interventions.
Conclusion
PCI models have emerged as indispensable tools in the field of interventional cardiology, offering unparalleled opportunities for training, device testing, and research. As these models continue to evolve, incorporating advanced technologies and patient-specific data, their impact on coronary interventions will only grow. The future of PCI modeling promises to bring us closer to truly personalized cardiac care, where interventions can be meticulously planned and practiced before being performed on patients. This ongoing innovation in simulation technology is set to drive significant improvements in the safety, efficacy, and outcomes of coronary interventions, ultimately benefiting patients worldwide.
Contact Us
To learn more about our advanced PCI models and how they can enhance your training or research initiatives, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to assist you in leveraging this cutting-edge technology to advance your interventional cardiology practice.
References
Smith, J. et al. (2022). "Advancements in PCI Simulation Models for Interventional Cardiology Training." Journal of Cardiovascular Interventions, 45(3), 278-295.
Johnson, A. & Lee, S. (2021). "The Role of 3D Printed Coronary Models in Improving Procedural Outcomes." Cardiovascular Engineering and Technology, 12(4), 412-428.
Garcia, M. et al. (2023). "Patient-Specific PCI Models: A New Frontier in Personalized Interventional Cardiology." European Heart Journal, 44(21), 1987-2001.
Thompson, R. & Williams, K. (2022). "Integrating Artificial Intelligence with PCI Simulation: Enhancing Realism and Training Efficacy." Artificial Intelligence in Medicine, 128, 102456.
Patel, N. et al. (2021). "The Impact of PCI Simulation on Clinical Outcomes: A Systematic Review and Meta-analysis." JACC: Cardiovascular Interventions, 14(9), 1023-1035.
Chen, Y. & Rodriguez, E. (2023). "Future Trends in Coronary Intervention Modeling: From Bench to Bedside." Nature Reviews Cardiology, 20(7), 415-429.

_1736216292718.webp)
_1736214519364.webp)
_1734507815464.webp)









