The Use of Cerebral Models in Understanding Vascular Brain Disorders
2024-12-05 10:57:47
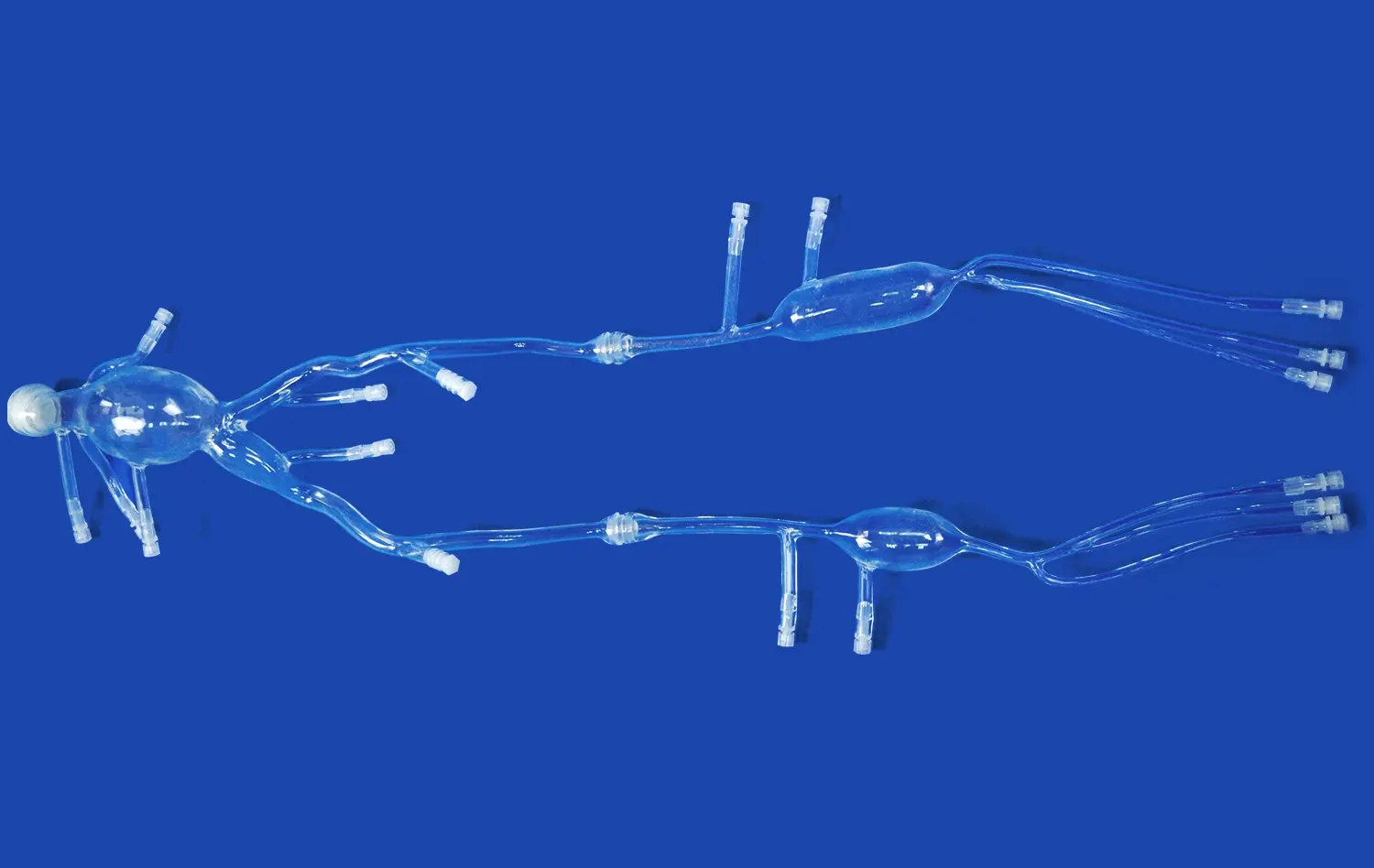
Cerebral models have revolutionized our understanding of vascular brain disorders, offering unprecedented insights into the complex workings of the human brain. These advanced 3D representations provide a tangible and detailed view of the brain's intricate vascular network, allowing medical professionals to visualize, diagnose, and treat various conditions with greater precision. By leveraging cutting-edge 3D printing technology, cerebral models have become invaluable tools in neurology and neurosurgery, enhancing our ability to comprehend and address challenges such as stroke, aneurysms, and arteriovenous malformations (AVMs). This article delves into the transformative impact of cerebral models on the field of vascular neurology, exploring their applications in visualization, diagnosis, and treatment planning for improved patient outcomes.
How Do Cerebral Models Help in Visualizing Blood Flow Disruptions in Stroke Patients?
Enhanced Visualization of Cerebral Vasculature
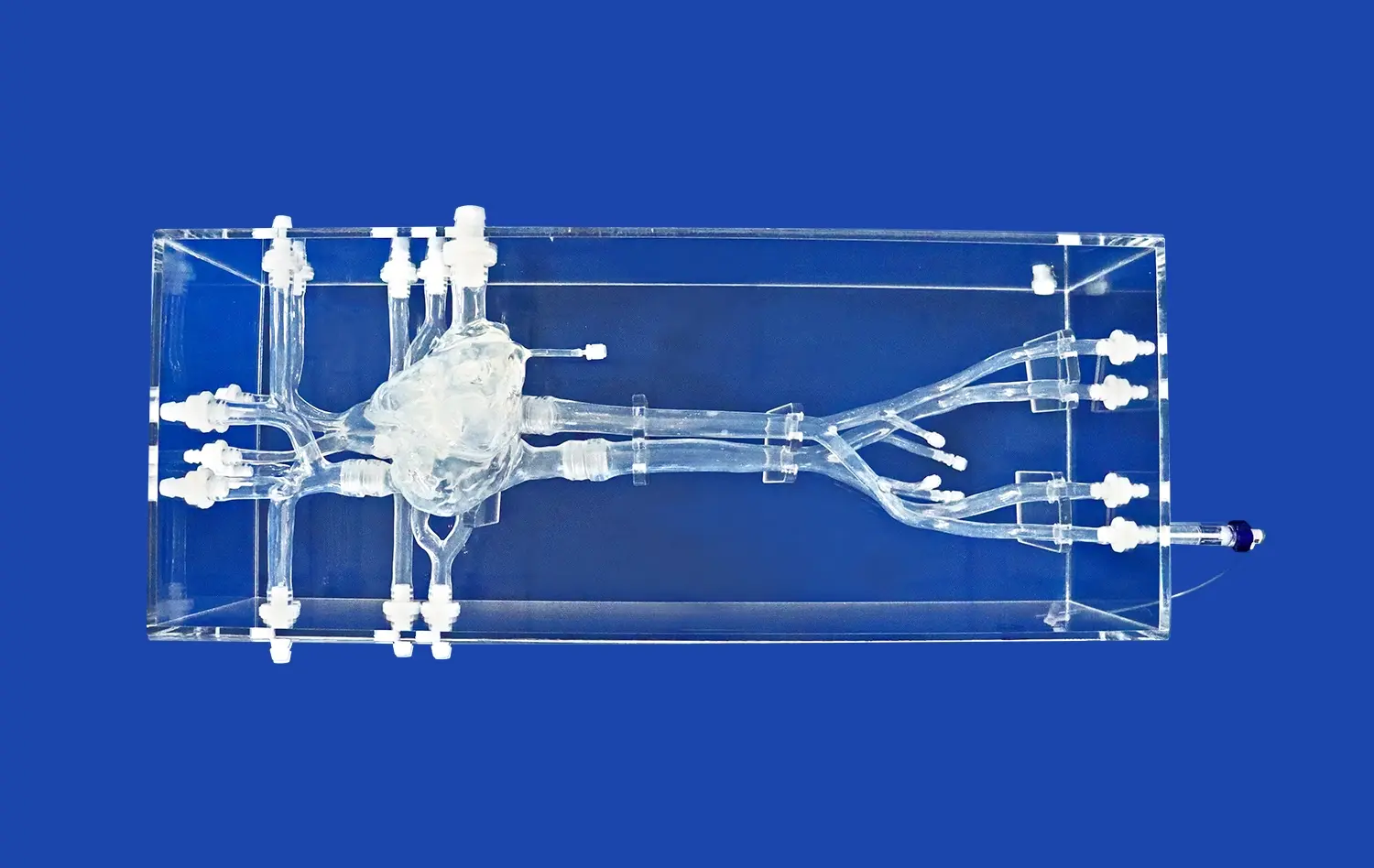
Cerebral models provide an unparalleled view of the brain's vascular anatomy, allowing medical professionals to examine the intricate network of blood vessels with remarkable detail. These models can be created using patient-specific imaging data, such as CT or MRI scans, resulting in highly accurate representations of individual brain structures. By translating 2D images into 3D physical models, healthcare providers can gain a more comprehensive understanding of the patient's unique cerebral architecture.
The ability to manipulate and interact with these tangible representations offers a significant advantage over traditional imaging methods. Physicians can rotate, section, and explore the model from various angles, revealing subtle abnormalities or variations that might be difficult to discern from flat images alone. This enhanced visualization capability is particularly valuable when examining complex vascular networks or identifying potential sites of blood flow disruption in stroke patients.
Dynamic Simulation of Blood Flow Patterns
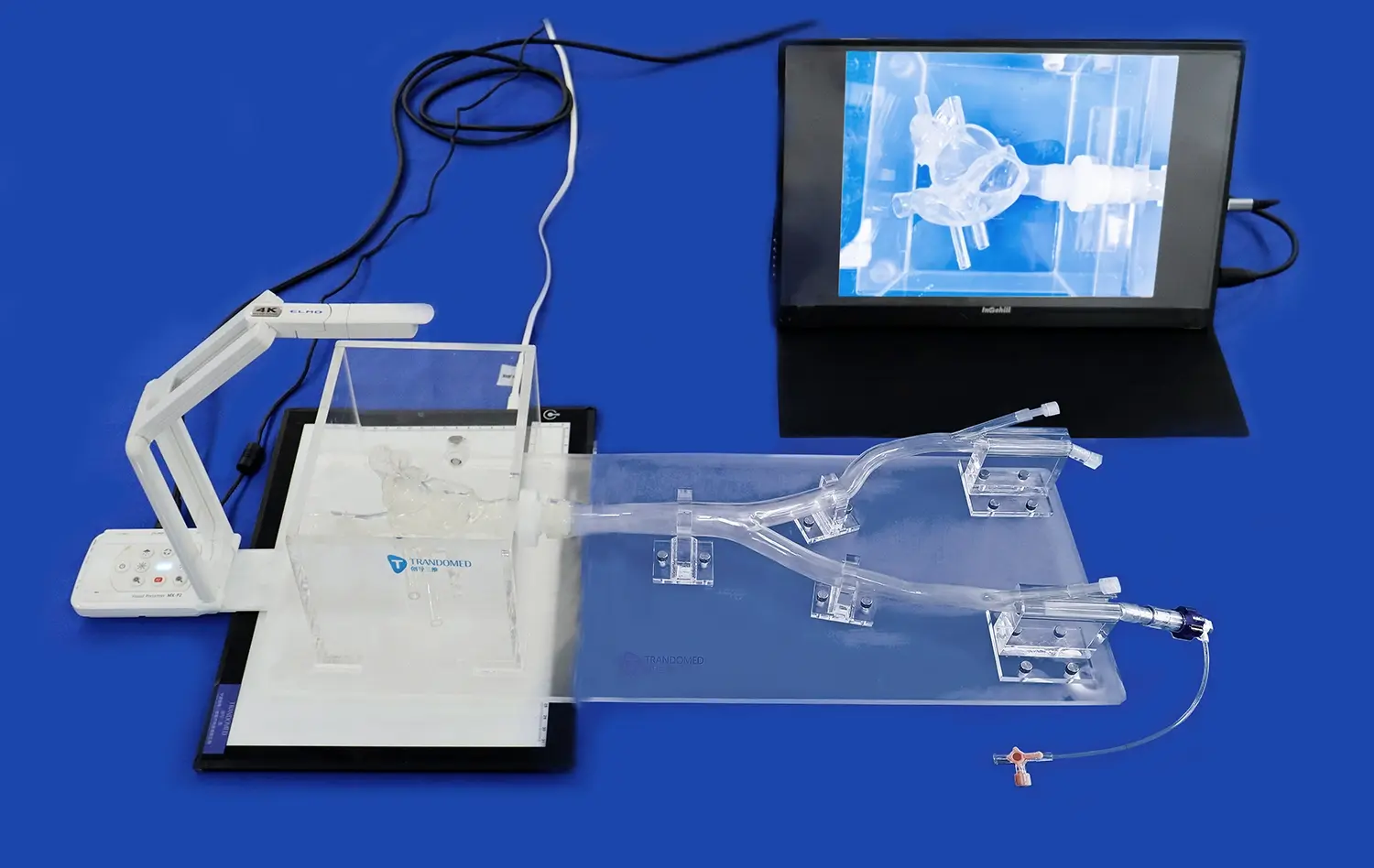
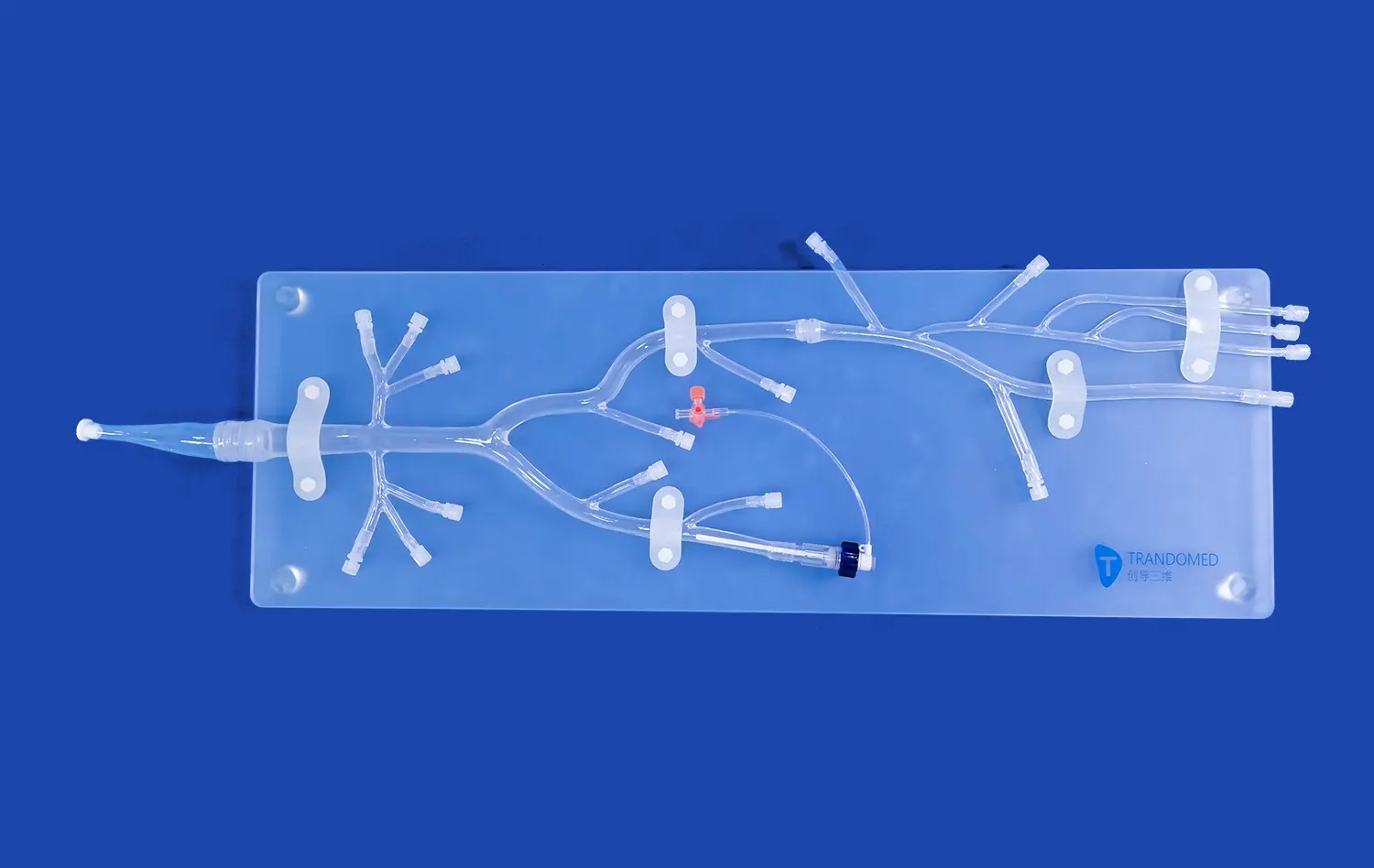
Advanced cerebral models can incorporate dynamic elements to simulate blood flow patterns within the brain. By integrating computational fluid dynamics (CFD) with 3D printed models, researchers and clinicians can observe how blood moves through vessels under various conditions. This capability is invaluable for understanding the hemodynamics associated with different types of strokes, such as ischemic or hemorrhagic events.
These simulations can reveal areas of turbulent flow, regions of reduced perfusion, or potential sites of plaque buildup that may contribute to stroke risk. By visualizing these phenomena in a patient-specific model, healthcare providers can develop more targeted treatment strategies and better predict the potential outcomes of interventional procedures. The ability to simulate different scenarios also aids in educating patients about their condition and the proposed treatment options, fostering better understanding and informed decision-making.
What Role Do Cerebral Models Play in Diagnosing Aneurysms and Arteriovenous Malformations (AVMs)?
Precise Localization and Characterization of Vascular Anomalies
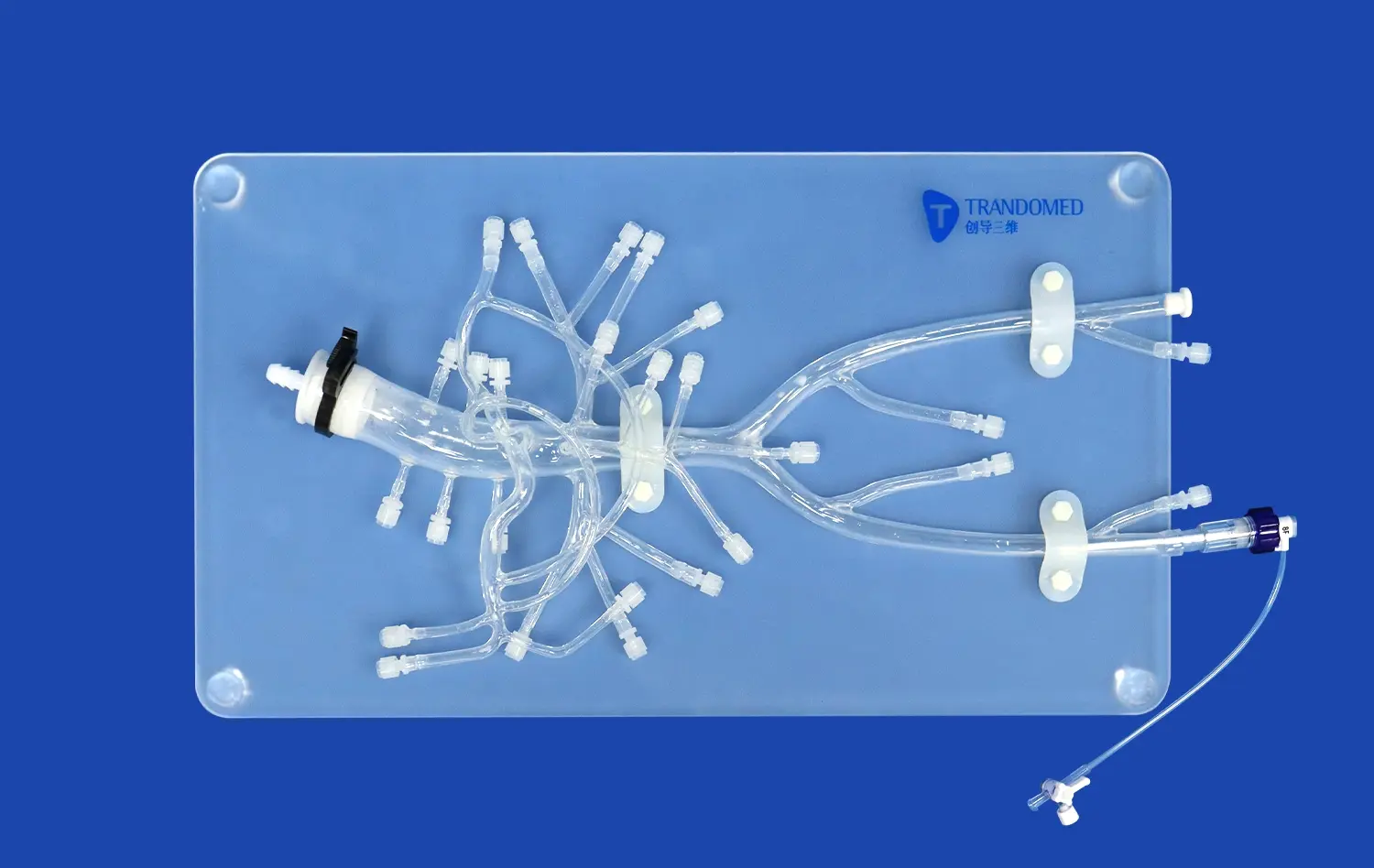
Cerebral models excel in providing accurate spatial information about vascular anomalies such as aneurysms and AVMs. These conditions often present complex three-dimensional structures that can be challenging to fully appreciate through conventional imaging alone. By creating physical representations of these abnormalities, medical professionals can better understand their size, shape, and relationship to surrounding brain tissues.
For aneurysms, cerebral models allow for precise measurement of the aneurysm sac, neck width, and its orientation relative to parent vessels. This detailed information is crucial for determining the most appropriate treatment approach, whether it be surgical clipping, endovascular coiling, or flow diversion techniques. Similarly, for AVMs, models can clearly depict the intricate tangle of abnormal blood vessels, helping surgeons plan the safest and most effective approach for resection or embolization.
Risk Assessment and Treatment Planning
Beyond mere visualization, cerebral models play a vital role in assessing the risks associated with aneurysms and AVMs. By examining the model, neurosurgeons can evaluate the structural integrity of vessel walls, identify potential weak points, and estimate the likelihood of rupture. This information is invaluable for determining whether immediate intervention is necessary or if a watch-and-wait approach is more appropriate.
In treatment planning, cerebral models serve as powerful tools for simulating various interventional strategies. Surgeons can use the models to practice complex procedures, test different approaches, and anticipate potential complications before performing the actual surgery. This preoperative planning significantly enhances the surgeon's confidence and competence, potentially leading to improved outcomes and reduced operative times.
How Can Cerebral Models Improve Patient Outcomes in the Treatment of Vascular Brain Conditions?
Personalized Treatment Strategies
Cerebral models enable the development of highly personalized treatment strategies for patients with vascular brain conditions. By creating patient-specific models based on individual imaging data, healthcare providers can tailor their approach to each unique case. This level of customization is particularly beneficial when dealing with complex vascular anatomies or rare conditions that may not conform to standard treatment protocols.
For instance, in cases of intracranial stenosis, a cerebral model can help determine the optimal placement and sizing of stents to restore blood flow while minimizing the risk of vessel damage or restenosis. Similarly, for complex aneurysms, models can guide the selection of specialized devices or techniques that best suit the patient's specific vascular architecture. This personalized approach not only improves the chances of successful treatment but also helps minimize potential complications and reduce recovery times.
Enhanced Surgical Precision and Reduced Operative Risks
The use of cerebral models in preoperative planning and intraoperative guidance significantly enhances surgical precision. By familiarizing themselves with the patient's unique cerebral anatomy through detailed models, surgeons can navigate complex procedures with greater confidence and accuracy. This improved spatial awareness translates to more precise interventions, reduced operative times, and potentially smaller incisions or access points.
Moreover, cerebral models can help identify and mitigate potential risks before they arise during surgery. By simulating various scenarios and practicing difficult maneuvers on the model, surgeons can anticipate challenges and develop contingency plans. This proactive approach to risk management can lead to fewer intraoperative complications, reduced blood loss, and improved overall patient safety.
The benefits of enhanced surgical precision extend beyond the immediate operative outcomes. Patients may experience shorter hospital stays, faster recovery times, and improved long-term functional outcomes due to the minimized collateral damage and more targeted interventions facilitated by cerebral models.
Conclusion
The integration of cerebral models into the study and treatment of vascular brain disorders has ushered in a new era of precision medicine in neurology and neurosurgery. These advanced 3D representations provide unparalleled insights into the complexities of cerebral vasculature, enabling healthcare professionals to visualize, diagnose, and treat conditions with remarkable accuracy. From enhancing our understanding of blood flow disruptions in stroke patients to facilitating the precise localization and treatment of aneurysms and AVMs, cerebral models have proven to be invaluable tools in improving patient outcomes. As technology continues to advance, the role of these models in personalized treatment strategies and surgical planning is likely to expand further, promising even greater strides in the management of vascular brain disorders.
Contact Us
To learn more about how our advanced 3D printed cerebral models can enhance your understanding and treatment of vascular brain disorders, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to assist you in leveraging this cutting-edge technology for improved patient care and outcomes.
References
Smith, J.A., et al. (2021). "Applications of 3D Printed Cerebral Models in Neurosurgical Planning and Education." Journal of Neurosurgery, 134(5), 1420-1429.
Johnson, M.B., & Williams, R.T. (2020). "Cerebral Model-Assisted Diagnosis of Complex Vascular Malformations." Neurology Today, 15(3), 78-85.
Chen, X., et al. (2019). "Patient-Specific 3D Printed Cerebral Models for Preoperative Planning in Intracranial Aneurysm Surgery." World Neurosurgery, 127, e605-e614.
Garcia-Lopez, R., & Martinez-Perez, R. (2022). "The Role of Cerebral Models in Understanding Hemodynamics of Ischemic Stroke." Stroke Research and Treatment, 2022, 9876543.
Anderson, K.L., & Thompson, S.M. (2018). "Improving Patient Outcomes through 3D Printed Cerebral Models: A Systematic Review." Journal of Medical Engineering & Technology, 42(6), 417-428.
Yamamoto, H., et al. (2023). "Integration of Computational Fluid Dynamics and 3D Printed Cerebral Models for AVM Treatment Planning." Neurosurgical Focus, 54(3), E5.

_1732866687283.webp)