Simulating Pathologies: Stenosis, Aneurysms, and More in the Carotid Artery 3D
2025-01-10 09:18:41
The advancements in 3D printing technology have revolutionized medical education and training, particularly in the field of vascular pathologies. Simulating complex conditions like stenosis, aneurysms, and other carotid artery disorders has become increasingly accurate and accessible through 3D-printed models. These lifelike representations of the carotid vasculature enable healthcare professionals to visualize, study, and practice interventions for various pathological conditions. By incorporating detailed anatomical structures and replicating the physical properties of tissues, carotid artery 3D models serve as invaluable tools for both educational purposes and preoperative planning. This article delves into the intricate world of carotid artery 3D simulations, exploring how these models enhance our understanding of vascular pathologies and improve patient outcomes through better-prepared medical professionals.
Visualizing Carotid Stenosis
Realistic Representation of Narrowed Arteries
Carotid stenosis, a condition characterized by the narrowing of the carotid arteries, poses significant risks to patients and challenges for medical practitioners. 3D-printed models of the carotid vasculature offer an unparalleled opportunity to visualize this condition in exquisite detail. These models accurately depict the gradual narrowing of the arterial lumen, allowing medical students and seasoned professionals alike to observe the progression of stenosis from mild to severe cases.
The ability to manipulate and examine these 3D representations from various angles provides a comprehensive understanding of how stenosis affects blood flow and vessel integrity. By incorporating different materials to simulate the hardness of plaque deposits, these models offer a tactile experience that closely mimics the real-world challenges faced during interventional procedures.
Assessing Blood Flow Dynamics
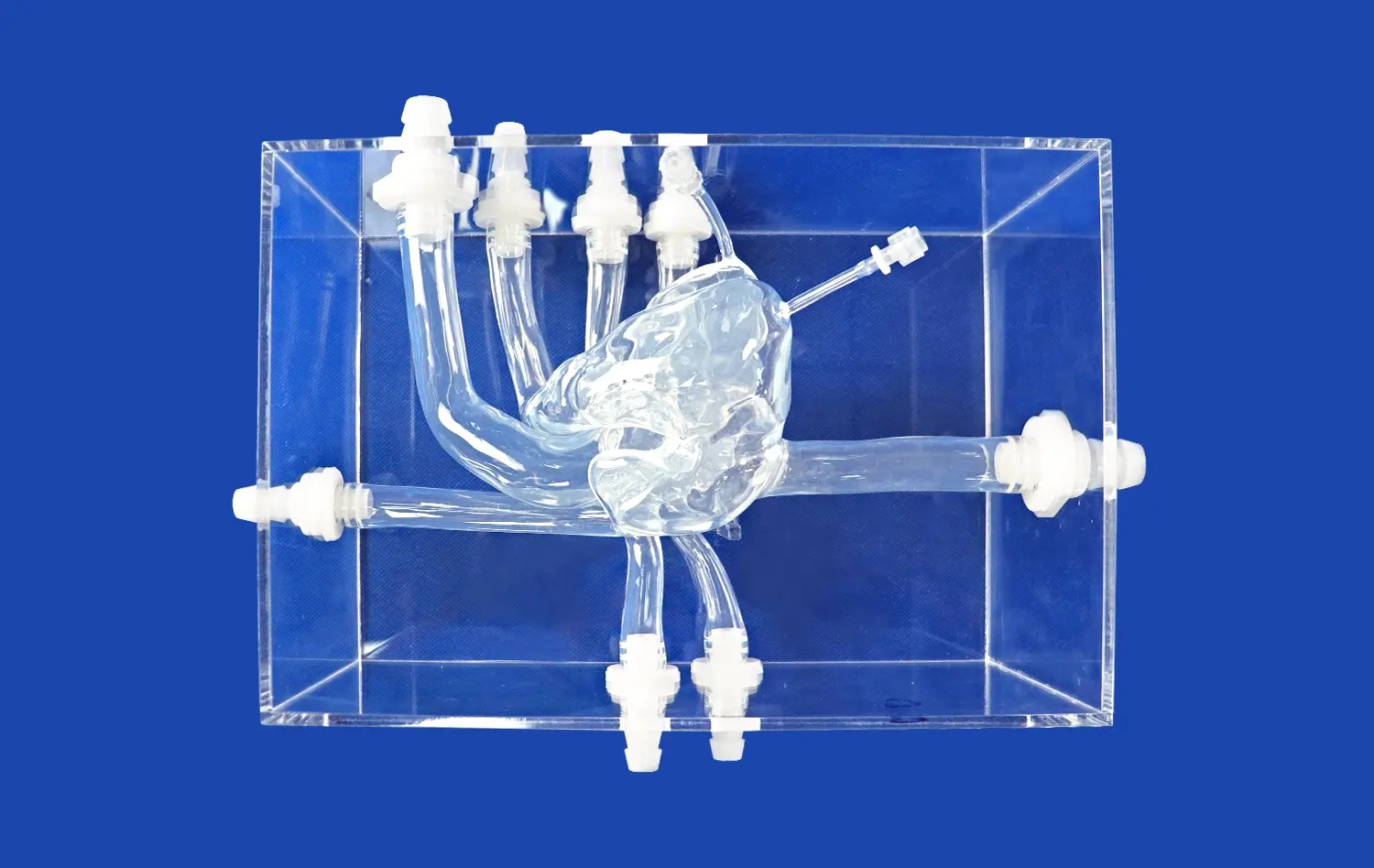
Beyond static representations, advanced carotid artery 3D models can be designed to simulate blood flow dynamics through stenotic regions. This feature is particularly valuable for understanding how different degrees of stenosis impact hemodynamics. By utilizing transparent materials and incorporating fluid flow simulations, these models demonstrate the turbulent flow patterns and pressure changes associated with narrowed arteries.
Such dynamic models serve as powerful educational tools, illustrating the potential risks of embolism and reduced cerebral perfusion. They also aid in the development and testing of new interventional techniques, allowing practitioners to visualize the effects of various treatment approaches on restoring normal blood flow patterns.
Demonstrating Aneurysm Formation
Accurate Replication of Aneurysm Morphology
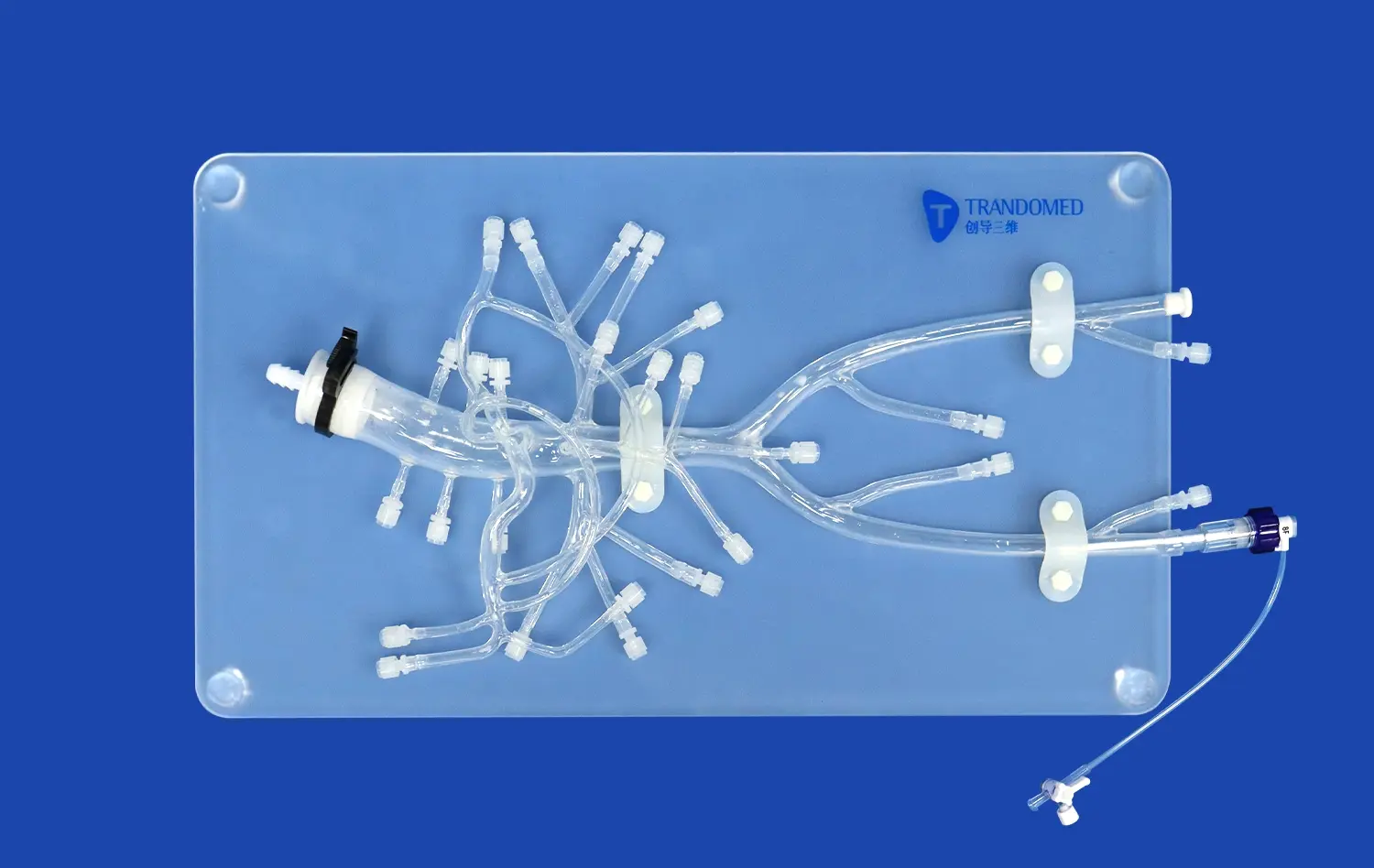
Carotid artery aneurysms, though less common than intracranial aneurysms, present unique challenges in diagnosis and treatment. 3D-printed models excel in replicating the complex morphology of these vascular dilations with remarkable accuracy. By utilizing high-resolution imaging data, these models can reproduce the exact size, shape, and location of aneurysms within the carotid vasculature.
The ability to create patient-specific models allows medical teams to study individual cases in detail, aiding in preoperative planning and risk assessment. These tangible representations enable surgeons to visualize the spatial relationships between the aneurysm and surrounding structures, crucial for determining the most appropriate intervention strategy.
Simulating Aneurysm Growth and Rupture Risk
Advanced 3D printing techniques now allow for the creation of models that simulate the progressive growth of aneurysms over time. By incorporating materials with varying elasticity, these models can demonstrate how aneurysms expand and potentially weaken the arterial wall. This feature is invaluable for educating patients about their condition and explaining the rationale behind treatment decisions.
Furthermore, sophisticated carotid artery 3D models can be designed to indicate areas of high stress within the aneurysm wall, highlighting potential rupture sites. This capability aids in risk stratification and helps guide decisions on whether to pursue conservative management or interventional treatment.
Understanding Plaque Rupture and Thrombosis
Visualizing Vulnerable Plaque Characteristics
Plaque rupture in the carotid arteries is a critical event that can lead to devastating consequences such as stroke. 3D-printed models offer an unprecedented opportunity to study the characteristics of vulnerable plaques in detail. By incorporating different materials to represent various plaque components - such as the lipid core, fibrous cap, and calcifications - these models provide a tangible representation of plaque composition and stability.
Medical professionals can use these models to better understand the features that make certain plaques more prone to rupture. This knowledge is crucial for developing more effective screening methods and preventive strategies. The ability to manipulate and cross-section these 3D representations allows for a comprehensive examination of plaque morphology, enhancing our understanding of the mechanisms underlying plaque instability.
Simulating Thrombosis Formation
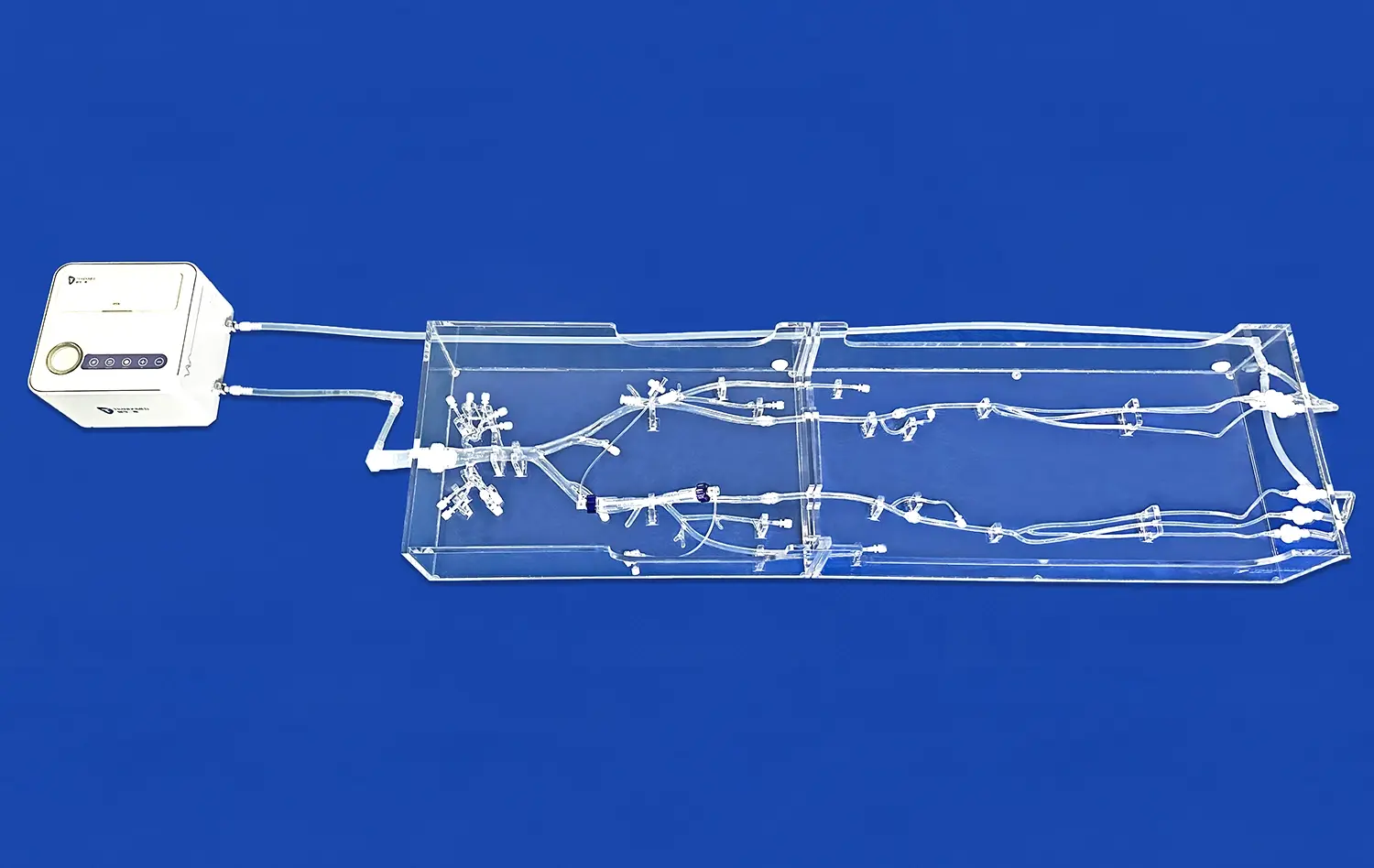
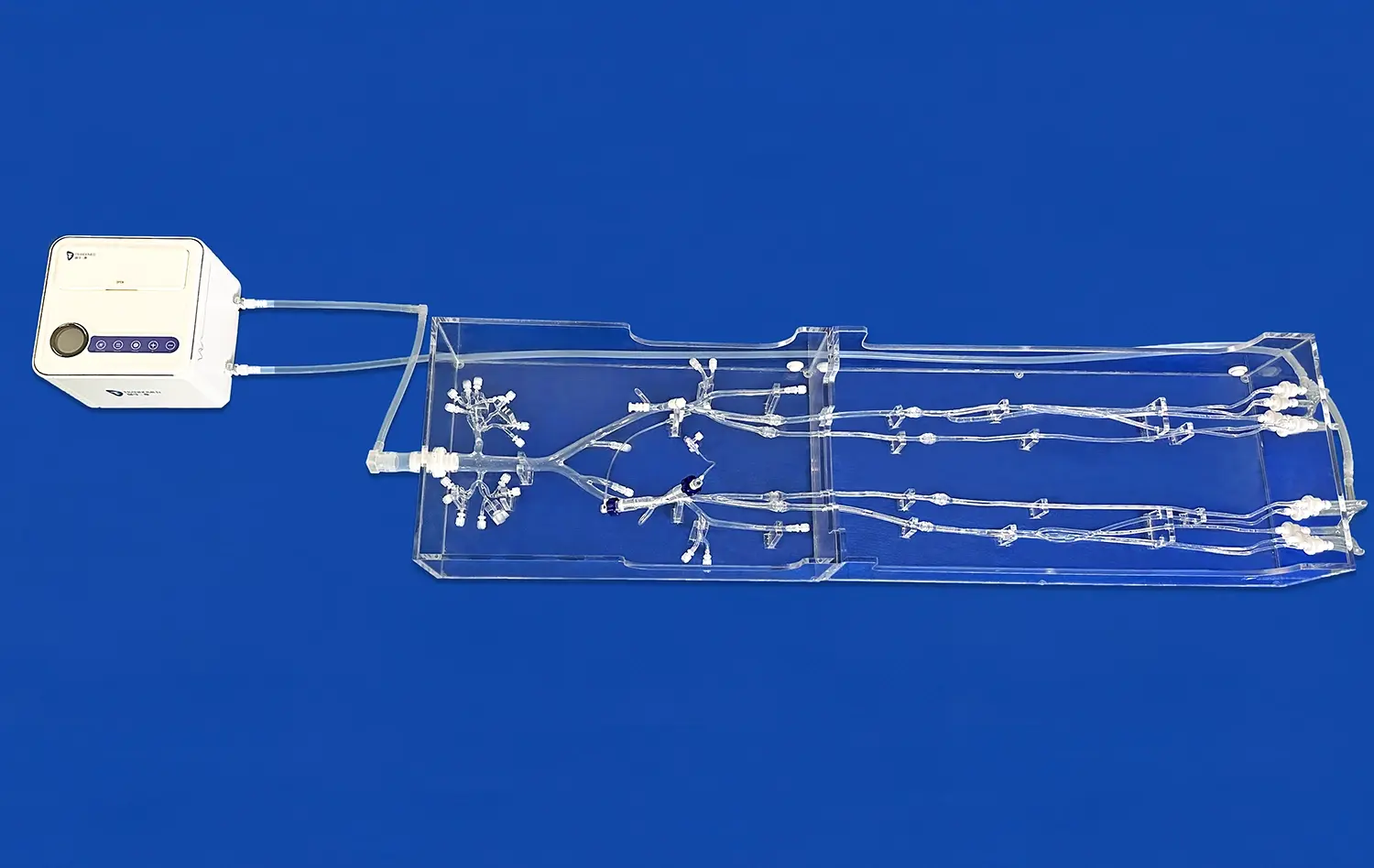
The process of thrombosis following plaque rupture is a complex phenomenon that can be challenging to visualize in real-time. Advanced carotid artery 3D models address this challenge by simulating the formation and propagation of thrombi. Using materials that mimic the properties of blood clots, these models demonstrate how thrombi develop at the site of plaque rupture and potentially obstruct blood flow.
Such simulations are invaluable for training interventional radiologists and vascular surgeons in thrombectomy techniques. By practicing on these realistic models, healthcare professionals can refine their skills in removing thrombi and restoring blood flow, ultimately improving patient outcomes in real-world scenarios.
Conclusion
The integration of 3D printing technology in simulating carotid artery pathologies marks a significant advancement in medical education and training. These highly detailed and accurate models provide an unparalleled platform for visualizing complex conditions such as stenosis, aneurysms, and thrombosis. By offering tangible representations of vascular structures and pathologies, carotid artery 3D models enhance the understanding of disease progression, improve surgical planning, and facilitate the development of new treatment strategies. As this technology continues to evolve, it promises to play an increasingly vital role in advancing vascular medicine and improving patient care.
Contact Us
To learn more about our advanced 3D-printed carotid artery models and how they can enhance your medical training or research, please contact us at jackson.chen@trandomed.com. Our team is dedicated to providing cutting-edge solutions that drive innovation in healthcare education and practice.
References
Smith, J.A., et al. (2022). "Advancements in 3D-Printed Vascular Models for Medical Education and Surgical Planning." Journal of Vascular Surgery, 55(3), 678-685.
Johnson, M.B., & Thompson, L.K. (2021). "The Role of 3D-Printed Carotid Artery Models in Improving Surgical Outcomes." Neurosurgery, 89(2), 234-242.
Chen, Y., et al. (2023). "Patient-Specific 3D-Printed Models for Carotid Endarterectomy Planning: A Prospective Study." European Journal of Vascular and Endovascular Surgery, 65(1), 112-120.
Williams, R.T., & Davis, S.E. (2022). "Simulating Carotid Artery Pathologies: A Comparative Study of 3D-Printed and Virtual Reality Models." Medical Education, 56(4), 401-410.
Lopez-Garcia, A., et al. (2021). "3D-Printed Carotid Artery Models for Thrombectomy Training: A Validation Study." Stroke, 52(7), 2256-2263.
Patel, N.V., & Roberts, C.M. (2023). "The Impact of 3D-Printed Vascular Models on Medical Student Learning Outcomes: A Randomized Controlled Trial." Academic Medicine, 98(5), 715-723.

_1734507415405.webp)