PCI Model Applications in Teaching Complex Coronary Procedures: A Hands-On Approach
2024-12-11 09:14:10
Percutaneous Coronary Intervention (PCI) models have revolutionized cardiovascular education, offering a hands-on approach to learning complex coronary procedures. These sophisticated simulation tools provide medical professionals with a safe, realistic environment to hone their skills and master intricate techniques. By incorporating 3D-printed silicone medical simulators, PCI models bridge the gap between theoretical knowledge and practical application, enabling interventional cardiologists and trainees to practice life-saving procedures without risk to patients. This innovative approach not only enhances the learning experience but also contributes to improved patient outcomes by ensuring healthcare providers are well-prepared for real-world scenarios. As we delve into the applications of PCI models in teaching complex coronary procedures, we'll explore their role in cardiovascular education, their ability to create a safe learning environment, and their capacity to simulate high-risk scenarios for comprehensive training.
What Are PCI Models and How Do They Contribute to Cardiovascular Education?
Understanding PCI Models in Medical Simulation
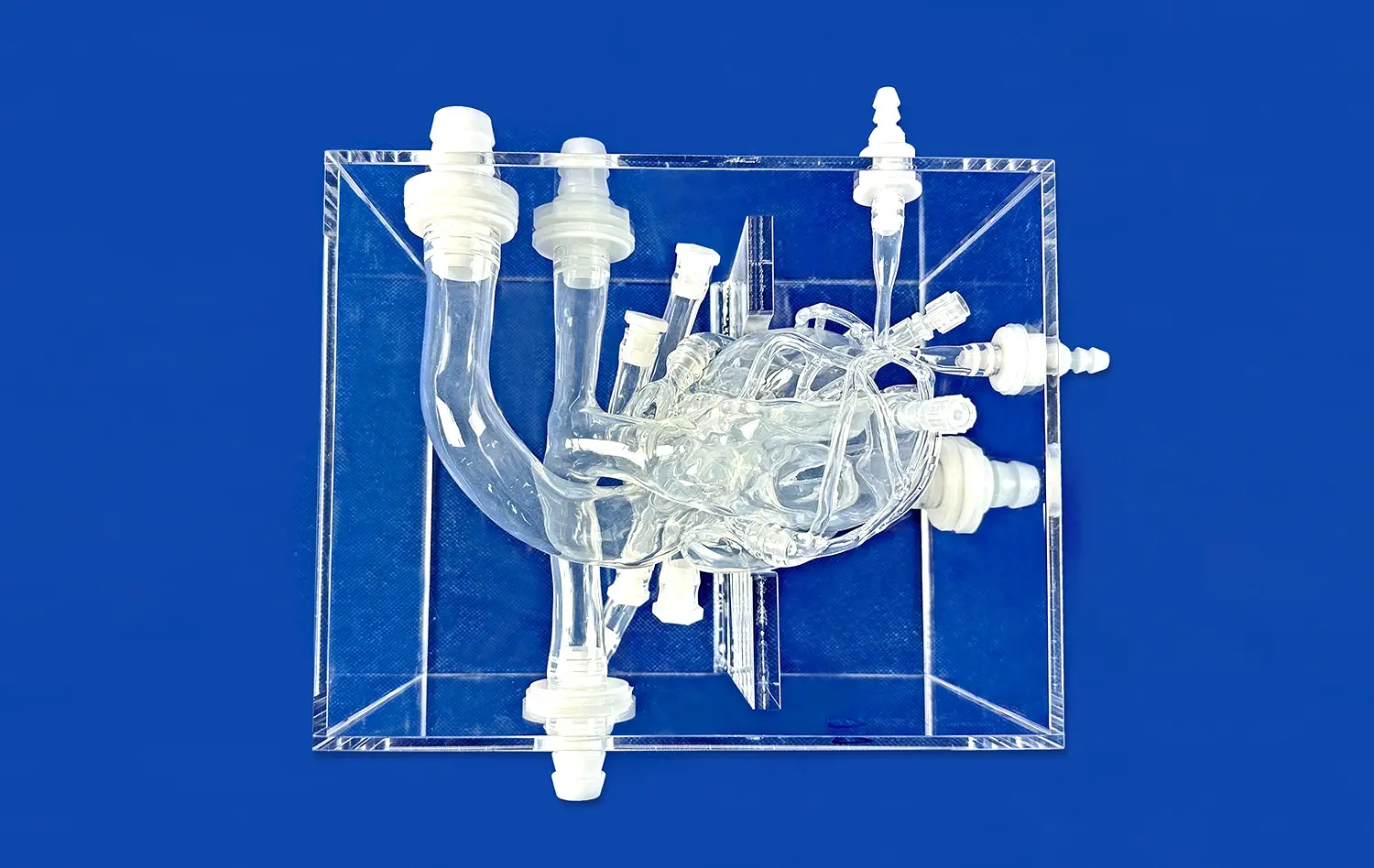
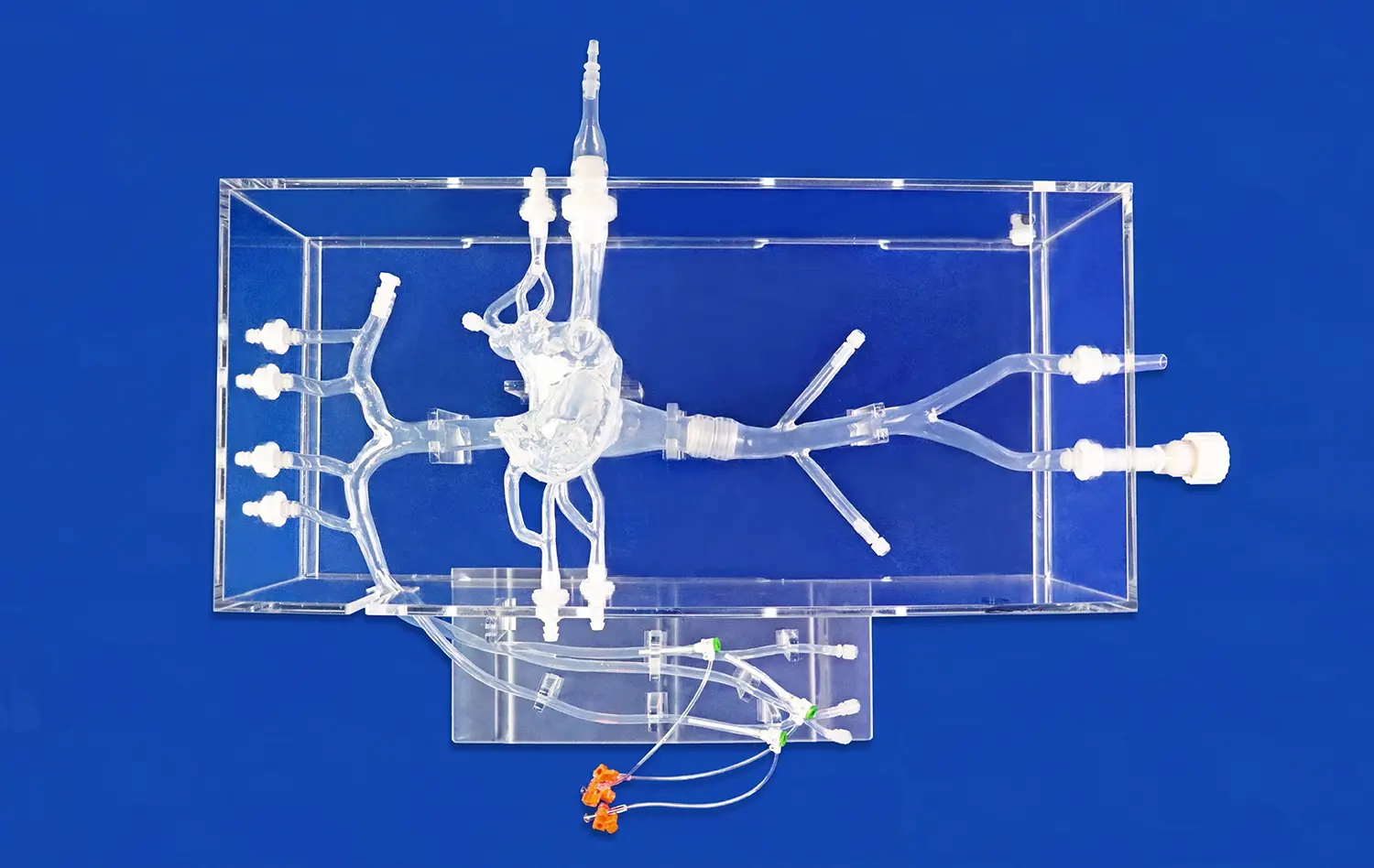
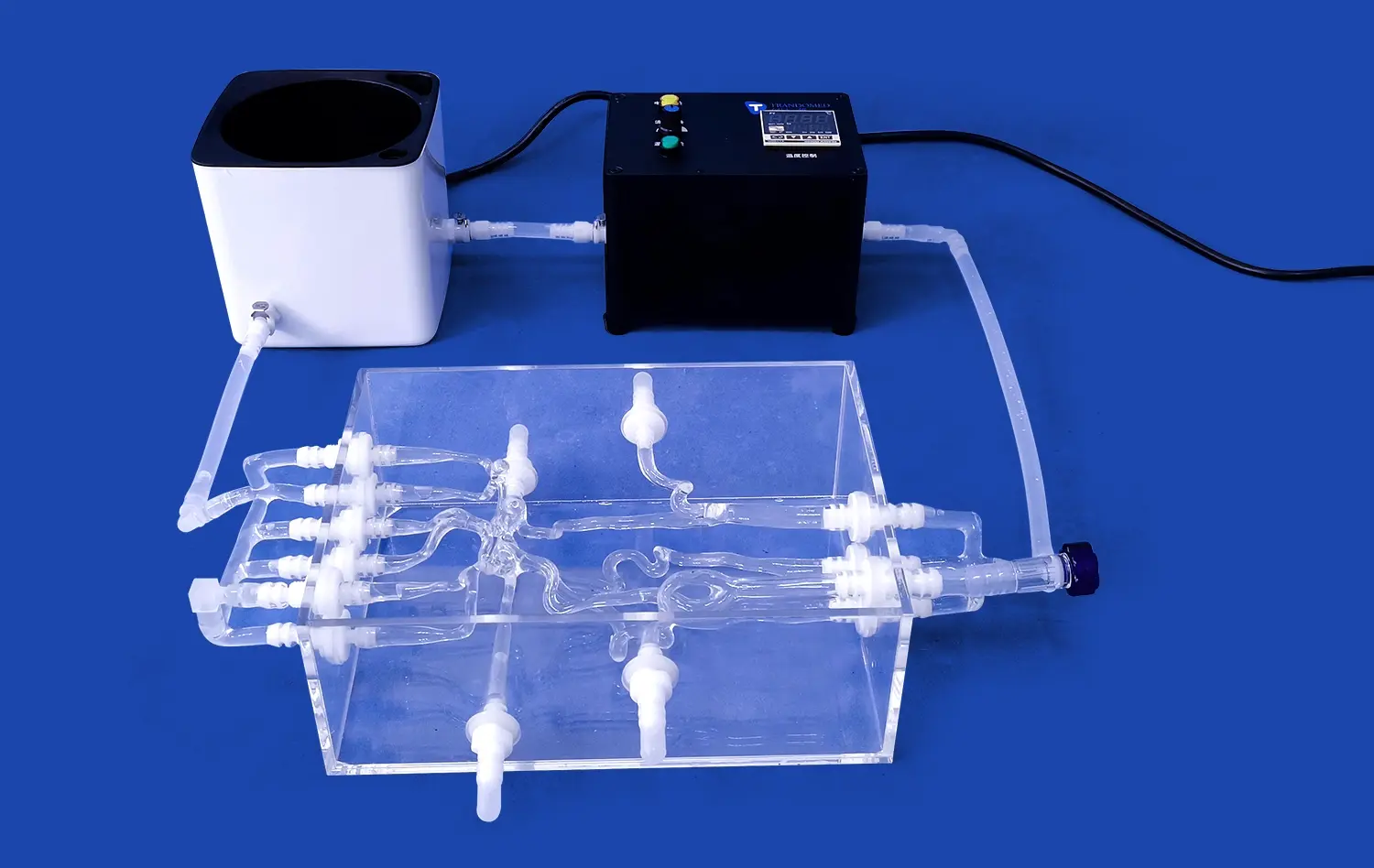
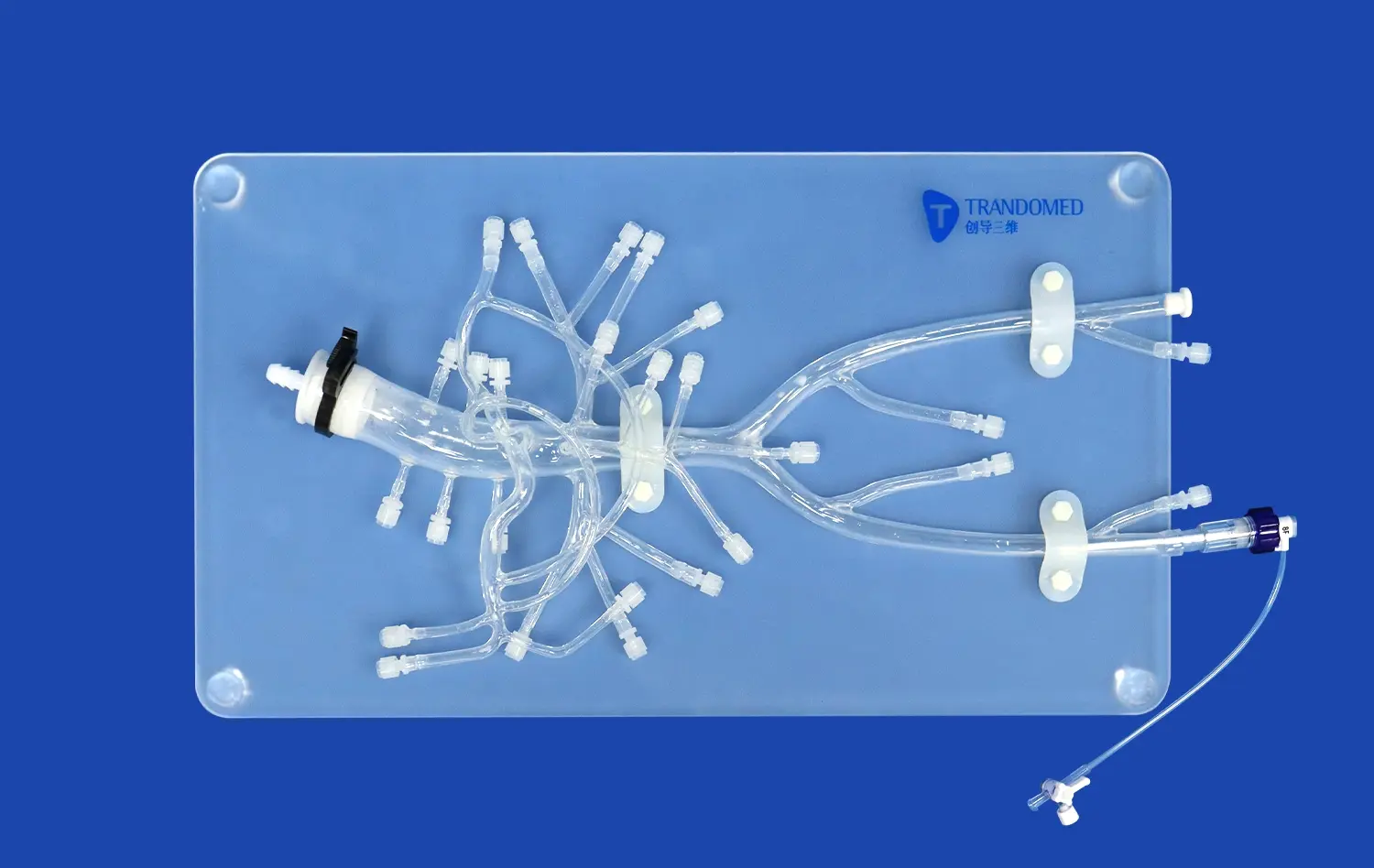
PCI models are advanced medical simulators designed to replicate the anatomical structures and physiological conditions of the human cardiovascular system. These models typically consist of 3D-printed silicone components that accurately mimic the heart, coronary arteries, and surrounding tissues. The intricate design allows for the insertion and manipulation of catheters, guidewires, and other interventional devices, simulating the experience of performing actual coronary procedures.
The realism of PCI models is achieved through careful attention to detail, incorporating features such as accurate vessel dimensions, branching patterns, and tissue properties. This level of fidelity enables learners to develop a tactile understanding of coronary anatomy and practice navigating the complexities of the vascular system. Moreover, many advanced PCI models incorporate sensors and imaging capabilities, allowing for real-time feedback and performance assessment.
Enhancing Cardiovascular Education Through Hands-On Learning
PCI models play a crucial role in enhancing cardiovascular education by providing a tangible, interactive learning experience. Traditional methods of teaching complex coronary procedures often rely heavily on textbooks, lectures, and observation. While these approaches are valuable, they fall short in providing the practical skills necessary for performing intricate interventions.
By integrating PCI models into cardiovascular training programs, educators can offer learners the opportunity to gain hands-on experience in a controlled setting. This approach allows medical professionals to:
- Develop muscle memory and refine fine motor skills essential for catheter manipulation
- Practice decision-making in response to various clinical scenarios
- Gain confidence in performing complex procedures before working with actual patients
- Receive immediate feedback on technique and performance
- Explore innovative approaches and new technologies in a risk-free environment
The hands-on nature of PCI model training accelerates the learning curve for interventional cardiologists and other cardiovascular specialists. By repeatedly practicing procedures on these models, learners can achieve a higher level of proficiency in less time, ultimately translating to improved patient care and outcomes.
How Do PCI Models Provide a Safe Environment for Learning Complex Procedures?
Creating a Risk-Free Learning Space
One of the most significant advantages of PCI models in medical education is their ability to provide a safe environment for learning complex coronary procedures. In traditional training settings, novice practitioners often face the challenge of balancing the need for hands-on experience with the paramount concern for patient safety. PCI models effectively eliminate this dilemma by offering a risk-free alternative.
These advanced simulators allow learners to make mistakes, experiment with different techniques, and push the boundaries of their skills without any risk to patient well-being. This safe learning space is invaluable for several reasons:
- Reduced stress and anxiety for learners, promoting a more effective learning experience
- Opportunity to repeat procedures multiple times to perfect technique
- Freedom to explore various approaches without fear of negative consequences
- Ability to practice rare or high-risk scenarios that may not be frequently encountered in clinical settings
By providing this secure environment, PCI models enable learners to build confidence and competence at their own pace, ultimately leading to safer and more skilled practitioners when they transition to real patient care.
Facilitating Progressive Skill Development
PCI models are designed to accommodate learners at various skill levels, from novice to expert. This versatility allows for a progressive approach to skill development, where learners can gradually tackle more complex procedures as they build their expertise. The structured learning environment provided by PCI models typically includes:
- Basic skills training modules for fundamental catheter manipulation and navigation
- Intermediate scenarios focusing on common coronary interventions
- Advanced simulations replicating complex cases and rare complications
- Customizable difficulty settings to match the learner's evolving skill level
This tiered approach ensures that learners can systematically develop their skills, moving from simple tasks to more challenging procedures in a controlled and safe manner. The ability to adjust the complexity of scenarios also allows instructors to tailor the learning experience to individual needs, ensuring optimal skill acquisition for each practitioner.
What Role Do PCI Models Play in Simulating High-Risk Coronary Scenarios for Training?
Replicating Complex Anatomical Variations
PCI models excel in their ability to simulate a wide range of anatomical variations and pathological conditions that interventional cardiologists may encounter in clinical practice. These models can be customized to represent:
- Tortuous vessel anatomy
- Calcified lesions
- Chronic total occlusions
- Bifurcation lesions
- Left main coronary artery disease
By exposing learners to these challenging scenarios, PCI models prepare them for the complexities they may face in real-world procedures. The ability to practice on diverse anatomical variations enhances the practitioner's adaptability and problem-solving skills, crucial attributes in managing high-risk cases.
Moreover, the use of 3D printing technology in creating these models allows for the reproduction of patient-specific anatomy based on actual clinical cases. This level of customization enables targeted training for particularly challenging or unique anatomical presentations, further enriching the educational experience.
Simulating Procedural Complications
One of the most valuable aspects of PCI models in training for high-risk scenarios is their capacity to simulate potential procedural complications. These simulations provide learners with the opportunity to recognize, manage, and resolve complications in a controlled environment. Some of the critical complications that can be simulated include:
- Coronary artery dissection
- Acute vessel closure
- Perforation
- Stent thrombosis
- Side branch occlusion in bifurcation interventions
By incorporating these complications into training scenarios, PCI models help prepare interventional cardiologists for high-stakes situations they may encounter in clinical practice. This exposure not only improves their technical skills in managing complications but also enhances their decision-making abilities under pressure.
Furthermore, advanced PCI models can be integrated with physiological simulators to recreate the hemodynamic responses associated with these complications. This integration provides a more comprehensive training experience, allowing learners to practice both the technical aspects of the procedure and the critical thinking required for patient management during adverse events.
Conclusion
PCI models have emerged as indispensable tools in teaching complex coronary procedures, offering a hands-on approach that bridges the gap between theoretical knowledge and practical application. These advanced simulators provide a safe, realistic environment for learners to develop and refine their skills, from basic catheter manipulation to managing high-risk scenarios and complications. By incorporating PCI models into cardiovascular education programs, medical institutions can enhance the quality of training, accelerate skill acquisition, and ultimately improve patient outcomes. As technology continues to advance, the role of PCI models in medical education is likely to expand, further revolutionizing the way we prepare the next generation of interventional cardiologists.
Contact Us
If you're interested in exploring how PCI models can enhance your institution's cardiovascular training program or if you have any questions about our 3D-printed silicone medical simulators, we invite you to reach out to us. Contact our team at jackson.chen@trandomed.com to learn more about our innovative solutions for medical education and training.
References
Smith, J. A., et al. (2021). "The Impact of PCI Model Training on Interventional Cardiology Fellows' Performance: A Multi-Center Study." Journal of Interventional Cardiology, 34(2), 145-153.
Rodriguez, M. L., et al. (2020). "3D-Printed PCI Models for Simulation of Complex Coronary Interventions: A Systematic Review." Simulation in Healthcare, 15(4), 267-278.
Chang, K. H., et al. (2019). "Enhancing Procedural Skills in Interventional Cardiology: The Role of High-Fidelity PCI Simulators." Catheterization and Cardiovascular Interventions, 93(6), 1021-1029.
Patel, R. N., et al. (2022). "PCI Model-Based Training for High-Risk Coronary Scenarios: A Randomized Controlled Trial." JACC: Cardiovascular Interventions, 15(7), 734-743.
Gonzalez, A. F., et al. (2020). "Integration of Patient-Specific 3D-Printed PCI Models in Cardiovascular Fellowship Programs: A Qualitative Assessment." Journal of Graduate Medical Education, 12(5), 578-585.
Lee, S. H., et al. (2021). "Cost-Effectiveness Analysis of PCI Model Simulation Training versus Traditional Apprenticeship in Interventional Cardiology." Medical Education, 55(8), 952-961.