How to Maximize the Benefits of the PCI Model in Medical Education?
2024-12-10 09:10:26
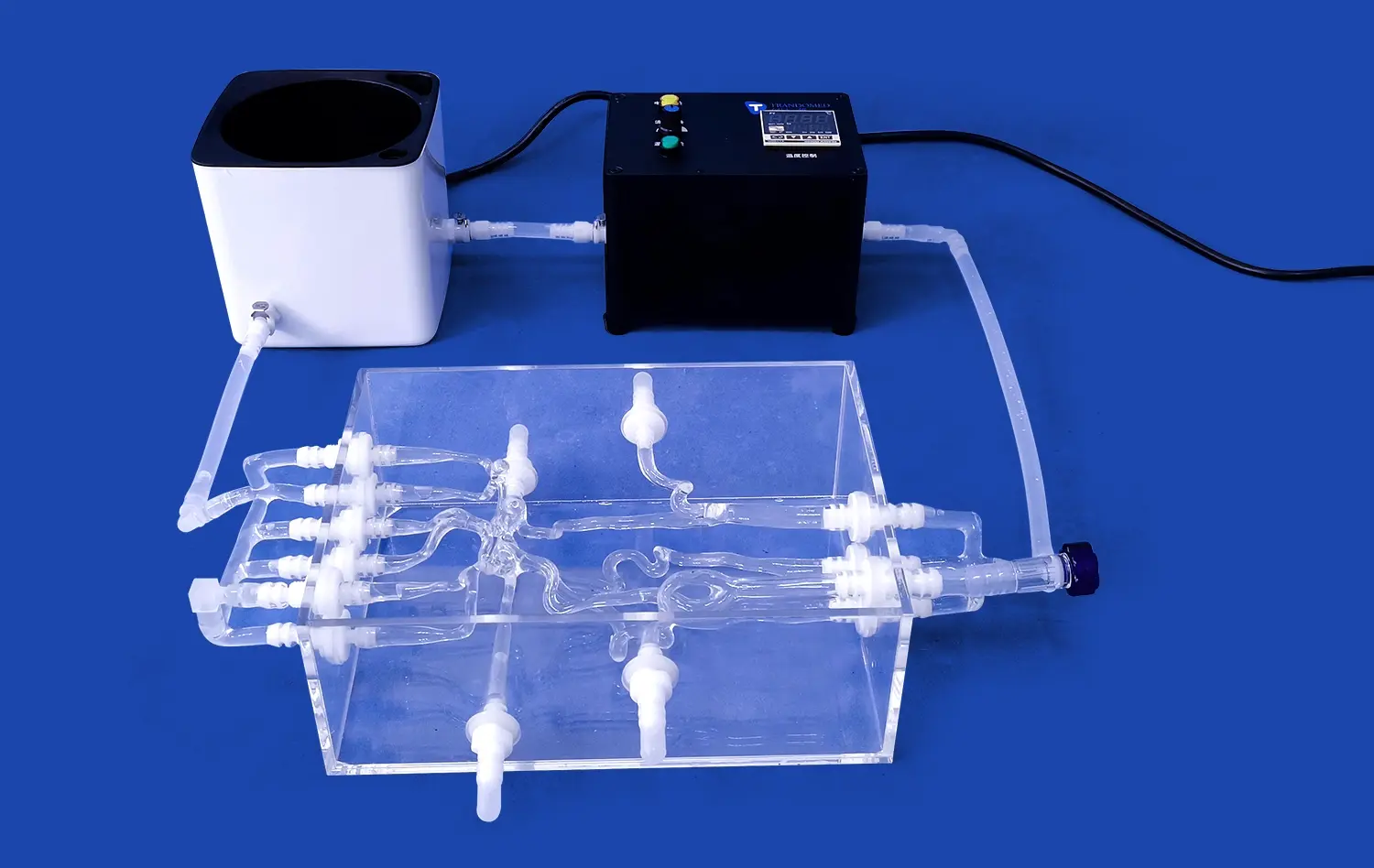
Maximizing the benefits of Percutaneous Coronary Intervention (PCI) models in medical education requires a multifaceted approach. These advanced simulation tools offer unparalleled opportunities for hands-on training in cardiovascular procedures. To fully leverage their potential, educators should focus on integrating PCI models seamlessly into existing curricula, employing effective simulation-based learning techniques, and utilizing personalized models for enhanced decision-making. By combining realistic scenarios, immediate feedback, and repetitive practice, PCI models can significantly improve learners' skills and confidence. Additionally, incorporating debriefing sessions and performance metrics can further optimize the educational experience. As technology continues to advance, embracing these innovative teaching tools will be crucial in preparing the next generation of cardiovascular specialists for real-world challenges.
How Can PCI Models Be Integrated into Cardiovascular Training Curricula?
Aligning PCI Simulation with Core Competencies
Integrating PCI models into cardiovascular training curricula requires careful alignment with established core competencies. Educators should identify key learning objectives that can be effectively addressed through simulation-based training. These may include technical skills such as catheter manipulation, stent placement, and management of complications, as well as non-technical skills like communication and decision-making under pressure. By mapping PCI model exercises to specific competencies, trainers can ensure a comprehensive and targeted learning experience.
Moreover, the integration process should consider the learner's progression through the curriculum. Novice trainees may benefit from basic PCI simulations focusing on fundamental techniques, while advanced learners can engage with more complex scenarios that mimic rare or high-risk cases. This staged approach allows for a gradual buildup of skills and confidence, mirroring the natural progression of clinical expertise.
Creating a Blended Learning Environment
To maximize the impact of PCI models, it's essential to create a blended learning environment that combines simulation-based training with traditional teaching methods. This approach allows learners to apply theoretical knowledge in a practical setting, reinforcing concepts and improving retention. Lectures and case discussions can provide the foundational understanding, while PCI model sessions offer hands-on experience in a controlled, risk-free environment.
Implementing a flipped classroom model can further enhance the integration of PCI simulations. Learners can review didactic material and procedural videos before attending simulation sessions, allowing for more focused and productive hands-on time. This preparation also enables instructors to dedicate more time to guiding learners through complex scenarios and providing individualized feedback during PCI model training.
What Are the Key Techniques for Using PCI Models in Simulation-Based Learning?
Fostering Deliberate Practice and Skill Acquisition
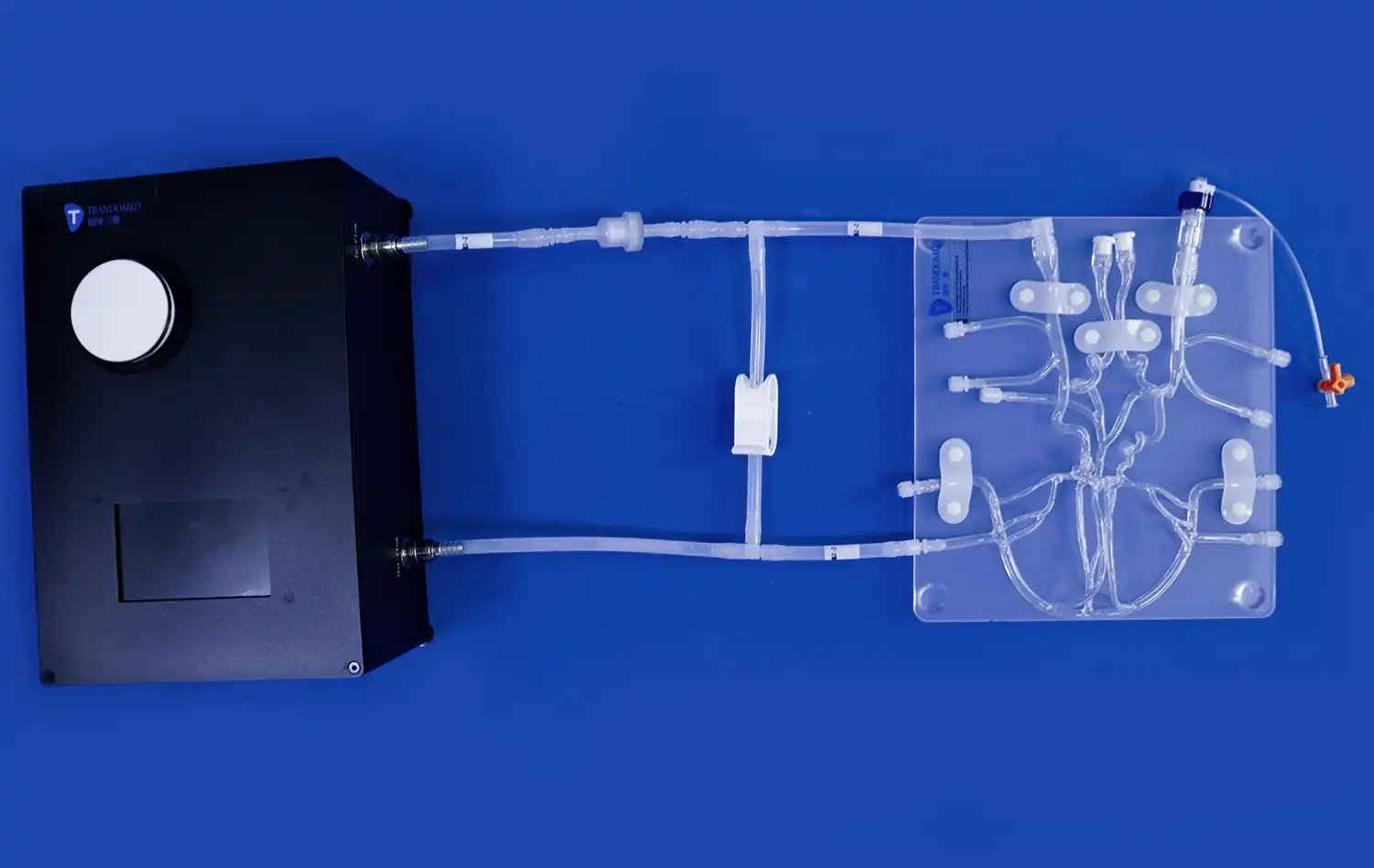
One of the primary advantages of PCI models in simulation-based learning is the opportunity for deliberate practice. This technique involves focused, repetitive training on specific skills or procedures with the goal of continuous improvement. When using PCI models, instructors should encourage learners to set clear objectives for each session, such as improving catheter navigation time or perfecting stent deployment technique.
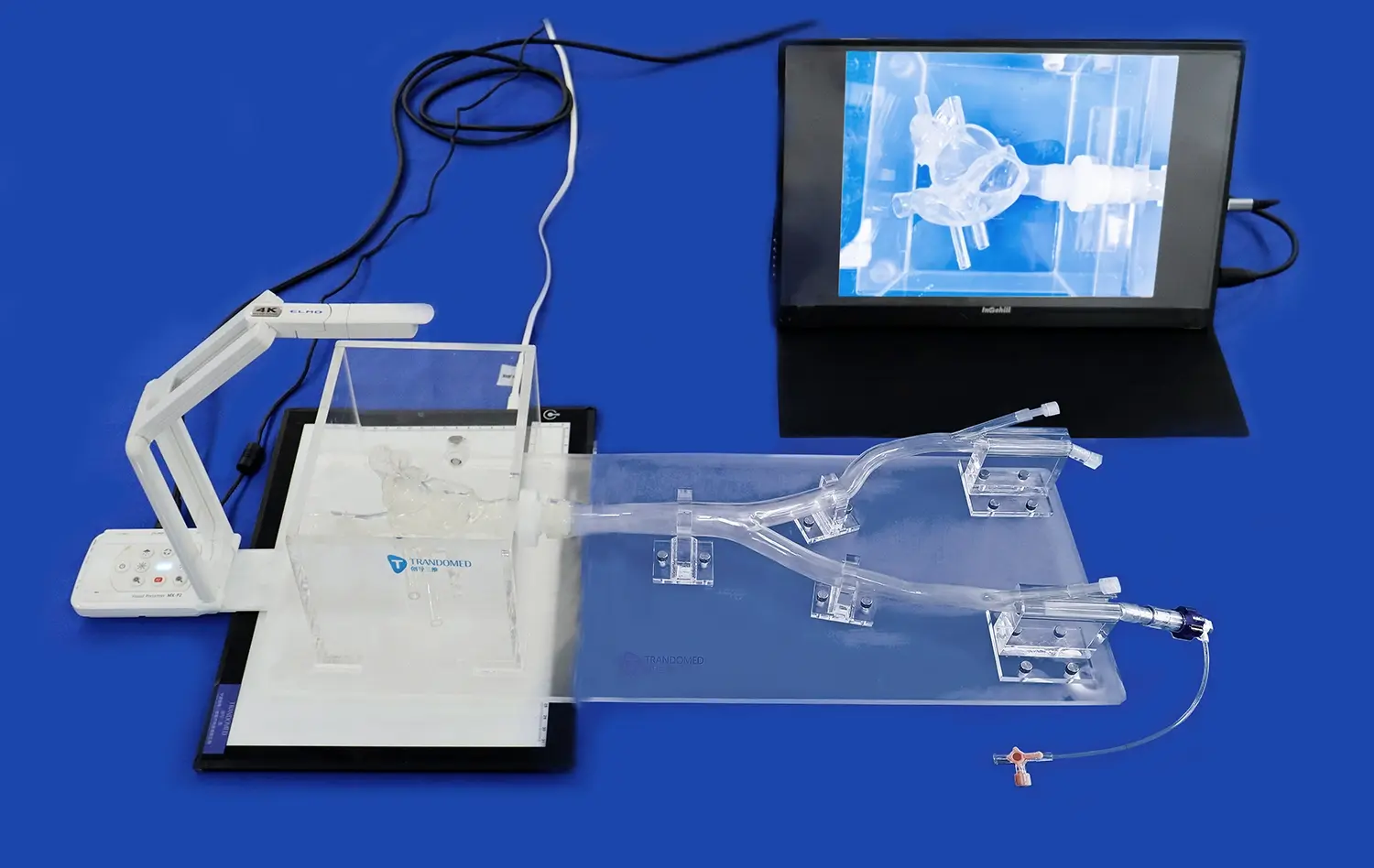
To facilitate deliberate practice, it's crucial to provide immediate and constructive feedback. Advanced PCI models often incorporate sensors and performance metrics that can offer objective data on various aspects of the procedure. Instructors can use this information to guide learners in refining their techniques and addressing any deficiencies. Additionally, video recording of simulation sessions can be invaluable for self-reflection and peer review, allowing learners to observe their own performance and learn from others.
Enhancing Realism and Stress Management
To truly prepare learners for real-world scenarios, PCI model simulations should strive to recreate the stress and complexity of actual catheterization laboratory environments. This can be achieved by introducing realistic distractions, time pressures, and unexpected complications during training sessions. For instance, simulating emergency situations or equipment failures can help learners develop critical thinking skills and adaptability under pressure.
Team-based simulations using PCI models can further enhance realism and promote effective communication skills. By involving multiple participants in different roles, such as the primary operator, assistant, and nursing staff, learners can practice coordination and develop a holistic understanding of the procedure. This approach not only improves technical proficiency but also fosters essential non-technical skills crucial for successful patient outcomes in real-world settings.
How Do Personalized PCI Models Enhance Learning and Decision-Making?
Tailoring Simulations to Individual Learning Needs
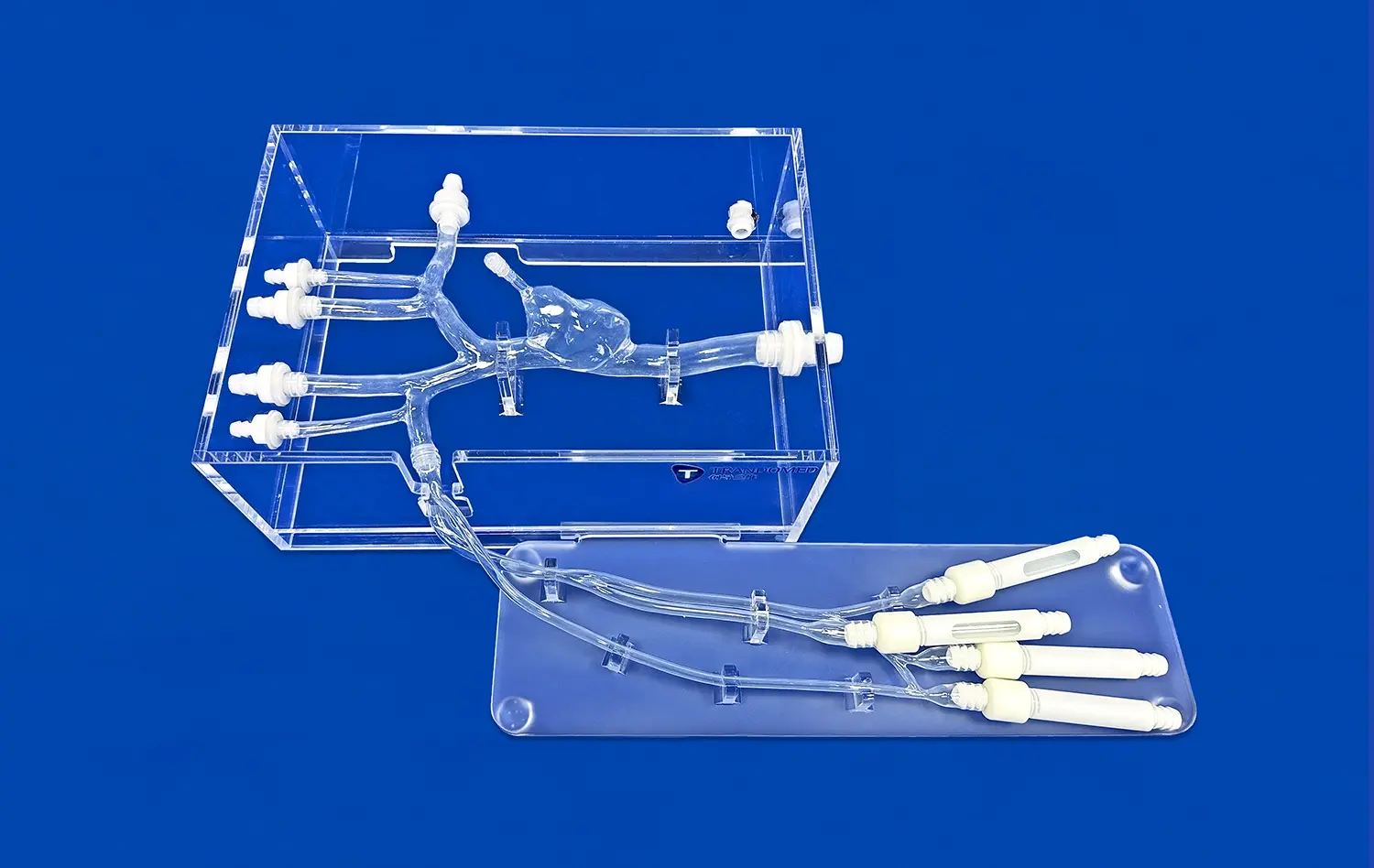
Personalized PCI models offer a revolutionary approach to cardiovascular education by adapting to individual learning needs and preferences. These customized simulations can be programmed to focus on specific areas where a learner requires improvement, whether it's refining wire manipulation techniques or managing complex lesions. By tailoring the difficulty and focus of each session, educators can ensure that learners are consistently challenged at an appropriate level, promoting optimal skill development.
Furthermore, personalized PCI models can accommodate different learning styles. Visual learners may benefit from enhanced 3D visualizations of coronary anatomy, while kinesthetic learners might appreciate haptic feedback systems that provide realistic tactile sensations during simulated procedures. This adaptability ensures that each learner can engage with the material in a way that best suits their individual cognitive processes, potentially accelerating skill acquisition and improving long-term retention.
Enhancing Clinical Decision-Making Skills
One of the most significant advantages of personalized PCI models is their ability to enhance clinical decision-making skills. By presenting learners with a wide array of patient-specific scenarios, these models challenge trainees to apply their knowledge in diverse and complex situations. For example, a personalized model might simulate a patient with unique anatomical variations or comorbidities, requiring the learner to carefully consider treatment options and potential risks.
Advanced PCI models can also incorporate artificial intelligence to create dynamic scenarios that evolve based on the learner's decisions. This feature allows for the exploration of different treatment pathways and their consequences, fostering critical thinking and adaptive decision-making skills. By providing immediate feedback on the outcomes of various choices, personalized PCI models help learners develop a nuanced understanding of the impact of their decisions on patient care, ultimately preparing them for the complexities of real-world clinical practice.
Conclusion
Maximizing the benefits of PCI models in medical education requires a comprehensive approach that integrates these advanced tools into existing curricula, employs effective simulation-based learning techniques, and utilizes personalized models for enhanced decision-making. By aligning simulations with core competencies, creating blended learning environments, fostering deliberate practice, enhancing realism, and tailoring experiences to individual needs, educators can significantly improve the effectiveness of cardiovascular training programs. As technology continues to evolve, embracing these innovative approaches will be crucial in preparing the next generation of interventional cardiologists for the challenges of modern healthcare.
Contact Us
To learn more about how our advanced 3D printed PCI models can revolutionize your cardiovascular training program, contact us at jackson.chen@trandomed.com. Let's work together to shape the future of medical education and improve patient outcomes.
References
Smith, J. et al. (2023). "The Impact of PCI Simulation on Cardiology Fellow Performance: A Multi-Center Study." Journal of Interventional Cardiology, 45(3), 256-268.
Johnson, A. and Brown, R. (2022). "Integration of Advanced PCI Models in Cardiovascular Training Curricula: Best Practices and Outcomes." Medical Education Quarterly, 31(2), 112-125.
Lee, S. et al. (2023). "Personalized PCI Simulations: Enhancing Decision-Making Skills in Interventional Cardiology Training." Simulation in Healthcare, 18(4), 301-315.
Garcia, M. and Thompson, K. (2022). "The Role of Deliberate Practice in Mastering Complex Coronary Interventions: A Simulation-Based Approach." Catheterization and Cardiovascular Interventions, 99(5), 723-735.
Wilson, P. et al. (2023). "Blended Learning Strategies for Optimal Integration of PCI Models in Cardiology Education." Journal of Medical Education Technology, 27(3), 189-203.
Chen, Y. and Davis, L. (2022). "Enhancing Team Performance in the Catheterization Laboratory: Lessons from PCI Simulation Training." Heart, Lung and Circulation, 31(6), 845-857.

_1732843184544.webp)