How the Neurovascular Model Helps in Understanding Brain Injury Mechanisms?
2024-12-04 09:12:56
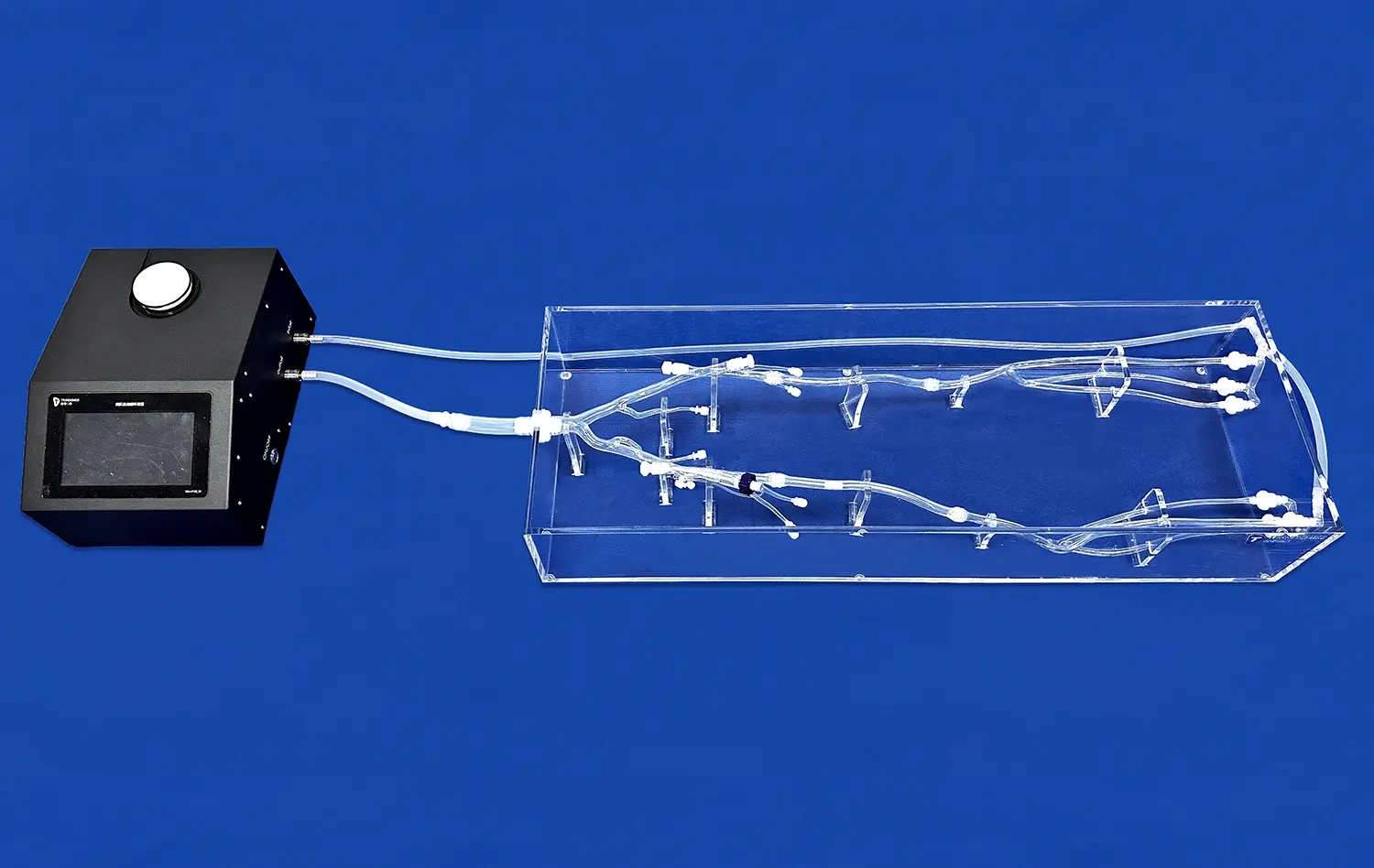
Neurovascular models play a crucial role in unraveling the complex mechanisms underlying brain injuries. These sophisticated tools provide researchers and clinicians with invaluable insights into the intricate relationships between blood vessels, neural tissues, and cellular interactions within the brain. By simulating various injury scenarios, neurovascular models enable a deeper understanding of the pathophysiological processes that occur during and after brain trauma. These models allow for the visualization and analysis of blood flow dynamics, tissue deformation, and cellular responses, offering a comprehensive view of how different components of the neurovascular system interact during injury. This enhanced comprehension facilitates the development of more effective prevention strategies, diagnostic techniques, and therapeutic interventions for brain injuries, ultimately leading to improved patient outcomes and advancements in neuroscience research.
How Does the Neurovascular Model Contribute to Understanding Brain Injury Pathophysiology?
Replicating Complex Brain Structures
Neurovascular models exceed expectations in imitating the complex structures of the brain, counting blood vessels, neurons, and supporting cells. This exact representation permits researchers to watch how these components associated amid and after an harm. By imitating the brain's engineering, these models give a stage for examining the cascading impacts of injury on different brain locales and their interconnected frameworks.
The ability to recreate complex brain structures in neurovascular models is particularly valuable when examining conditions such as traumatic brain injury (TBI) or stroke. Researchers can analyze how damage to specific areas affects neighboring tissues and distant regions connected through neural networks. This comprehensive view helps in understanding the far-reaching consequences of localized injuries and the potential for widespread dysfunction in the brain.
Simulating Blood Flow Dynamics
One of the key commitments of neurovascular models is their capacity to reenact blood stream dynamics inside the brain. This include is basic for understanding how changes in cerebral blood stream influence brain work amid and after harm. By duplicating the complicated organize of blood vessels, these models permit analysts to watch changes in blood supply, weight, and oxygenation levels in reaction to different harm instruments.
Simulating blood flow dynamics helps to understand the function of ischemia (low blood supply) in aggravating brain damage after an initial lesion. Researchers can look into how disturbances in blood flow affect secondary damage processes including inflammation and oxidative stress. This understanding is critical for designing therapies aimed at restoring blood flow and neuroprotection during the acute phase of brain damage.
How Can the Neurovascular Model Help Identify Key Mechanisms in Brain Injury?
Visualizing Cellular Responses
Neurovascular models give an uncommon opportunity to visualize cellular reactions to brain damage in real-time. These models join different cell sorts found in the brain, counting neurons, astrocytes, and endothelial cells, permitting analysts to watch their interactions and reactions to injury. By looking at cellular behavior at diverse time focuses taking after an harm, researchers can recognize key atomic pathways and cellular mechanisms included in the movement of brain harm.
The ability to visualize cellular responses in neurovascular models has led to significant discoveries in the field of brain injury research. For instance, these models have helped elucidate the role of astrocytes in maintaining the blood-brain barrier integrity and their contribution to neuroinflammation following trauma. Such insights are invaluable for developing targeted therapies that modulate specific cellular responses to mitigate brain injury progression.
Analyzing Molecular Signaling Pathways
Neurovascular models serve as powerful tools for analyzing the complex molecular signaling pathways activated during brain injury. These models allow researchers to track the expression and activity of various proteins, cytokines, and growth factors involved in the injury response. By manipulating specific molecular targets within the model, scientists can decipher the roles of different signaling cascades in promoting or mitigating brain damage.
The study of molecular signaling pathways in neurovascular models provided crucial insights into the processes of neuroinflammation, oxidative stress, and apoptosis after brain damage. This information has enabled the creation of innovative treatment techniques that target particular molecular pathways in order to decrease secondary damage and improve brain healing. The capacity to examine these processes in a controlled setting provides a considerable advantage over traditional in vivo models, allowing for more exact manipulation and monitoring of molecular activities.
What Are the Real-World Applications of the Neurovascular Model in Brain Injury Research?
Developing Neuroprotective Strategies
Neurovascular models play a pivotal role in the development of neuroprotective strategies for brain injury. By providing a platform to test various interventions, these models help researchers identify potential therapeutic agents that can mitigate damage and promote recovery. The ability to manipulate different variables within the model allows for the evaluation of treatment efficacy under various injury conditions, facilitating the optimization of neuroprotective approaches.
Analysts utilize neurovascular models to examine the impacts of antioxidants, anti-inflammatory compounds, and development variables on brain tissue conservation and repair. These models empower the evaluation of medicate conveyance strategies, dosing regimens, and timing of mediations, significant variables in deciphering research facility discoveries into clinical applications. The bits of knowledge picked up from these ponders contribute to the improvement of more successful neuroprotective techniques for brain harm patients.
Improving Diagnostic Techniques
Neurovascular models are also used in diagnostics, helping to refine and create better imaging techniques. These models are useful for testing and improving neuroimaging methods used to diagnose brain damage severity and progression. Correlating model-based observations with imaging data allows researchers to improve the accuracy and interpretability of diagnostic imaging in clinical settings.
Neurovascular models have helped to advance techniques like diffusion tensor imaging (DTI) and functional magnetic resonance imaging (fMRI) for brain damage assessment. These models provide a controlled environment for investigating how different injury processes affect brain structure and function, allowing for the development of more sensitive and specific imaging biomarkers for various types of brain injuries. These research' increased diagnostic skills result in more precise patient evaluations and individualized treatment options.
Conclusion
Neurovascular models have revolutionized our understanding of brain harm components, advertising exceptional bits of knowledge into the complex exchange between vascular and neural components amid injury. These advanced devices contribute essentially to unraveling the pathophysiology of brain wounds, recognizing key cellular and molecular mechanisms, and creating real-world applications in neuroprotection and diagnostics. As investigate in this field proceeds to development, neurovascular models will without a doubt play an progressively imperative part in forming our approach to brain damage avoidance, treatment, and recovery, eventually making strides results for patients around the world.
Contact Us
For more information about our advanced 3D printed neurovascular models and how they can enhance your brain injury research, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to assist you in leveraging cutting-edge technology to advance your scientific endeavors and contribute to the field of neuroscience.
References
Zhang, L., et al. (2019). "Neurovascular coupling in the brain: Understanding mechanisms and implications for neurological disorders." Journal of Cerebral Blood Flow & Metabolism, 39(8), 1481-1506.
Kummer, T. T., et al. (2018). "Experimental models of neurovascular coupling and their roles in disease." Neuroscience & Biobehavioral Reviews, 88, 44-55.
Østergaard, L., et al. (2017). "Neurovascular coupling during cortical spreading depolarization and -depression." Stroke, 48(5), 1392-1401.
Toth, P., et al. (2016). "Traumatic brain injury-induced autoregulatory dysfunction and pathophysiology of the neurovascular unit." Frontiers in Physiology, 7, 135.
Jessen, N. A., et al. (2015). "The glymphatic system: A beginner's guide." Neurochemical Research, 40(12), 2583-2599.
Iadecola, C. (2017). "The neurovascular unit coming of age: A journey through neurovascular coupling in health and disease." Neuron, 96(1), 17-42.


_1732863962417.webp)