How PCI Models Are Used in Patient-Specific Planning for Coronary Interventions?
2024-12-12 10:24:47
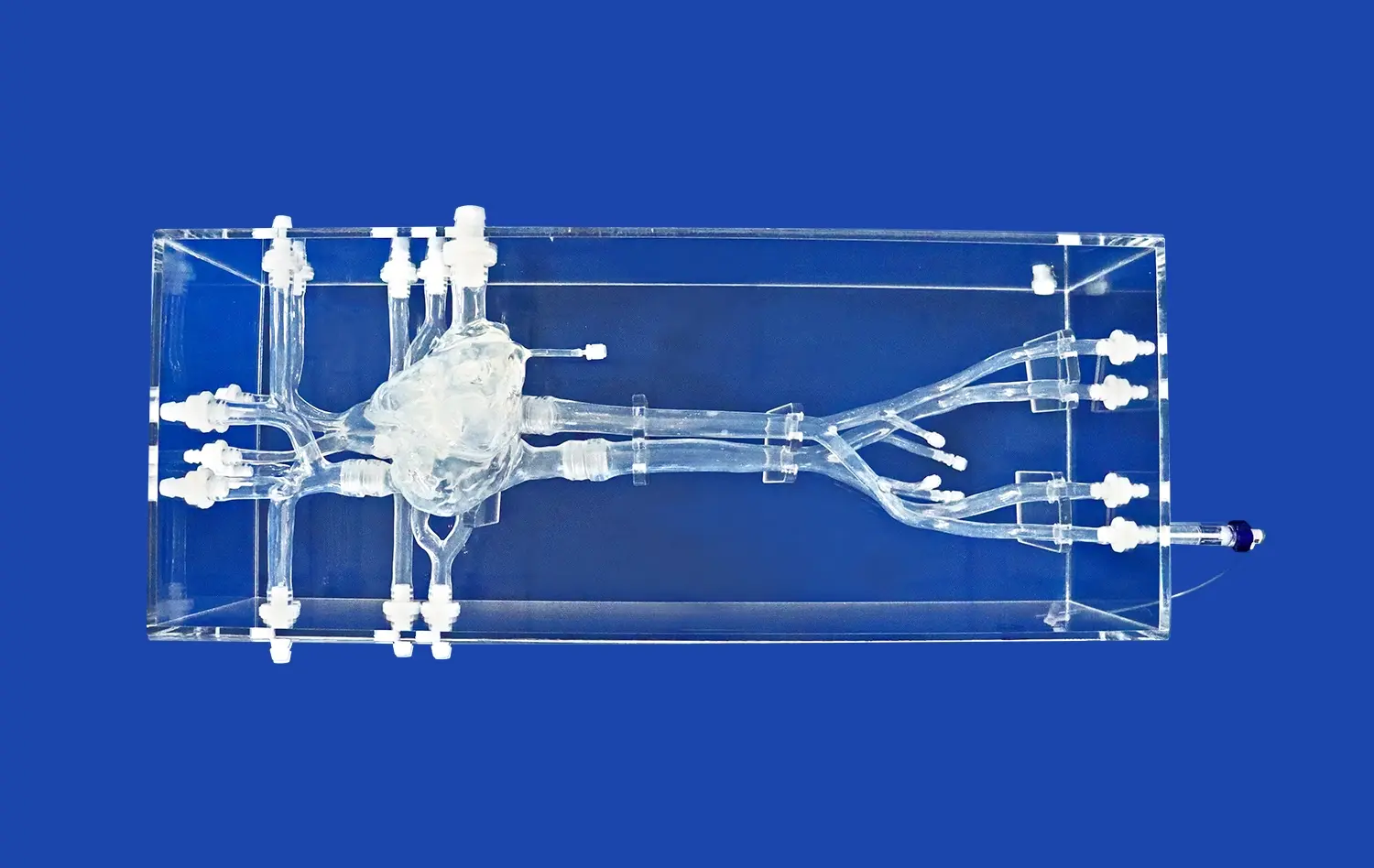
Patient-specific planning for coronary interventions has been revolutionized by the advent of PCI (Percutaneous Coronary Intervention) models. These advanced 3D printed simulations, derived from patient-specific imaging data, offer cardiologists an unprecedented level of insight into individual coronary anatomy and pathology. By providing a tangible, highly accurate representation of a patient's heart and coronary arteries, PCI models enable interventional cardiologists to meticulously plan and rehearse complex procedures before entering the catheterization laboratory. This approach not only enhances procedural efficiency but also significantly improves patient outcomes by allowing for personalized treatment strategies. The use of PCI models in pre-procedural planning has become an invaluable tool in navigating the intricacies of coronary interventions, particularly in cases involving complex lesions or anatomical variations.
How Do PCI Models Help Cardiologists Plan Complex Coronary Interventions?
Enhancing Visualization and Understanding of Coronary Anatomy
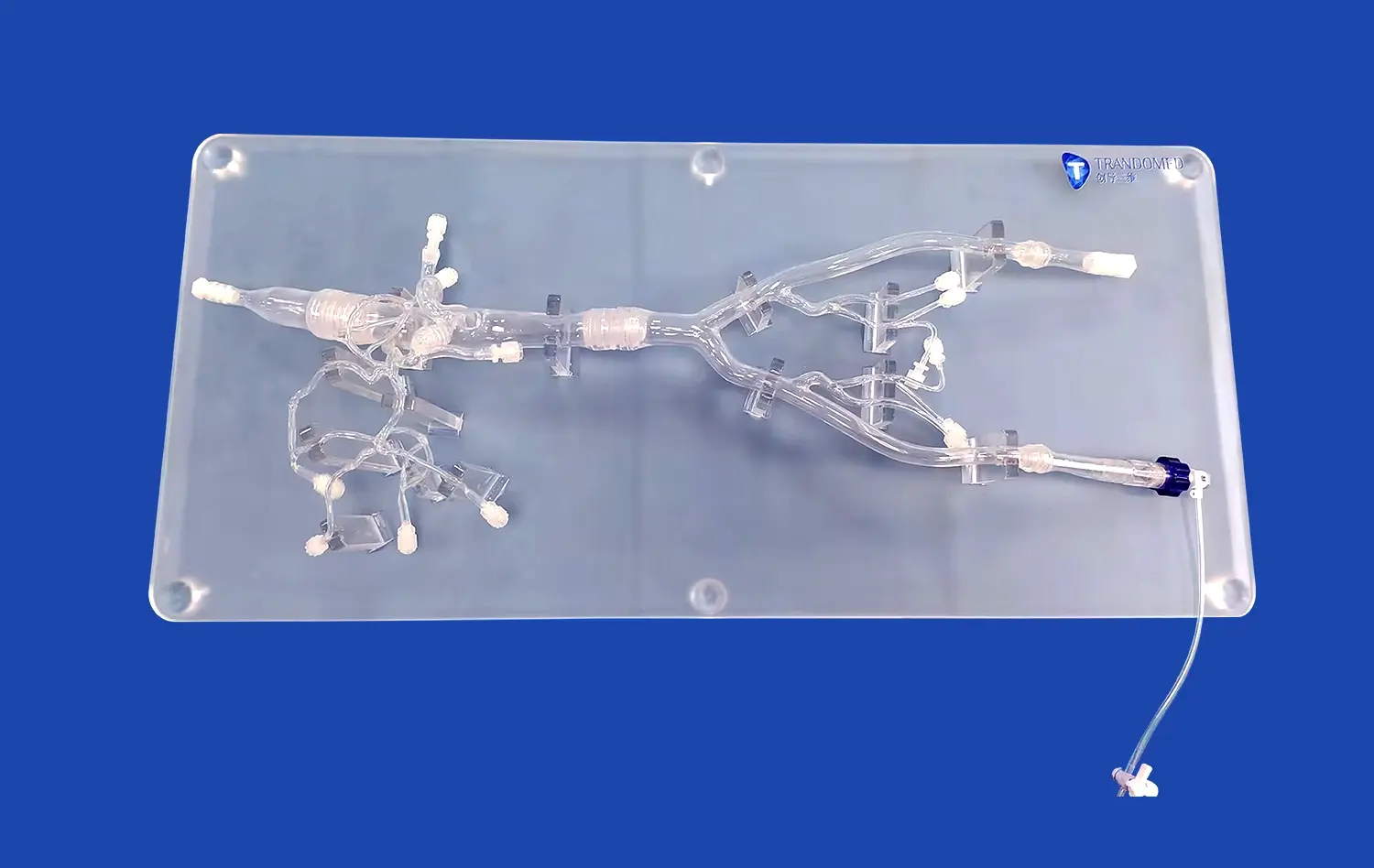
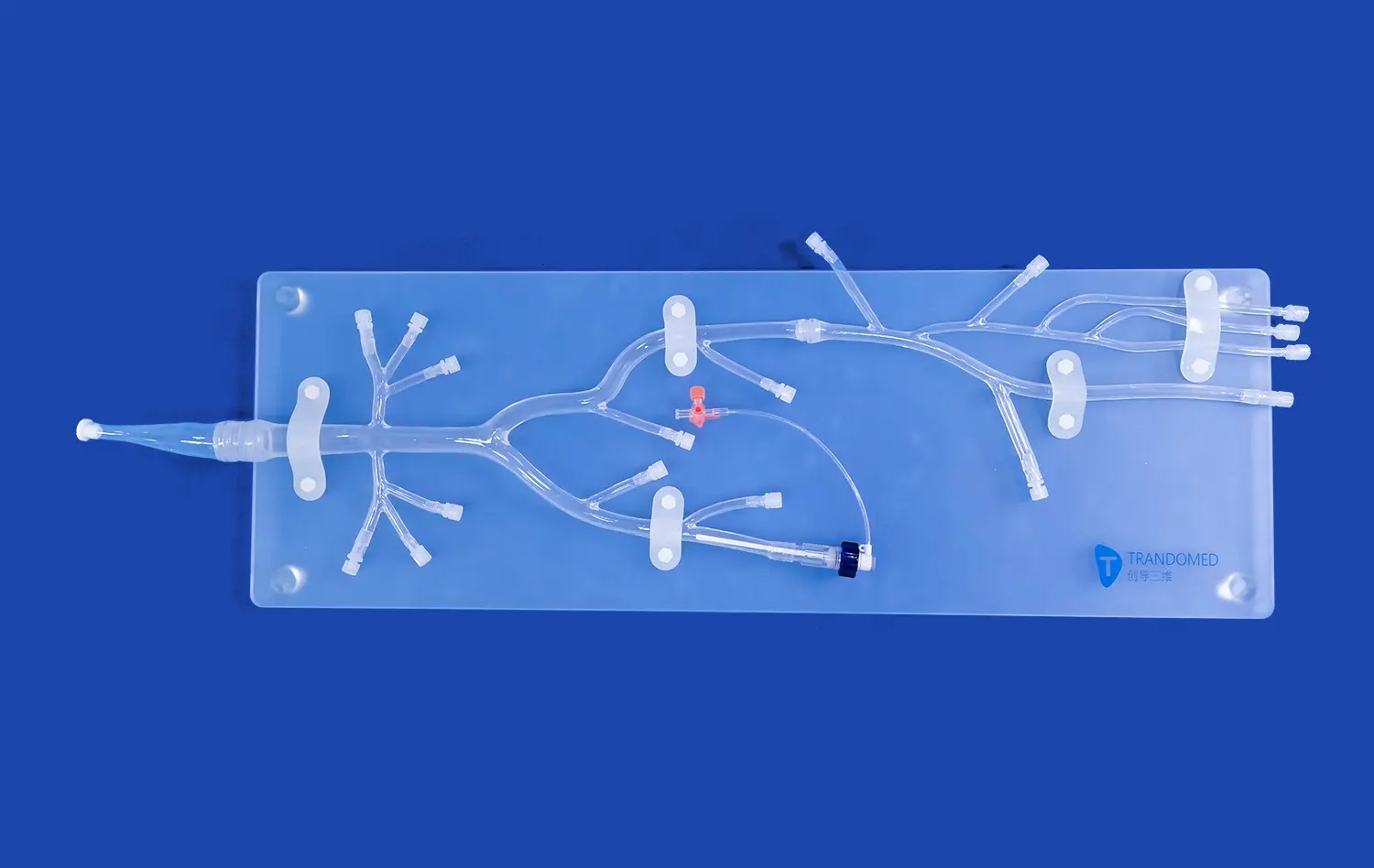
PCI models provide cardiologists with a three-dimensional representation of a patient's coronary arteries, offering a level of detail and perspective that traditional imaging methods cannot match. This enhanced visualization allows interventionalists to fully appreciate the unique anatomical features of each patient's coronary tree, including vessel tortuosity, bifurcation angles, and the spatial relationships between different arterial segments. By manipulating the physical model, cardiologists can examine the coronary anatomy from multiple angles, gaining insights that might be missed when relying solely on two-dimensional angiographic images.
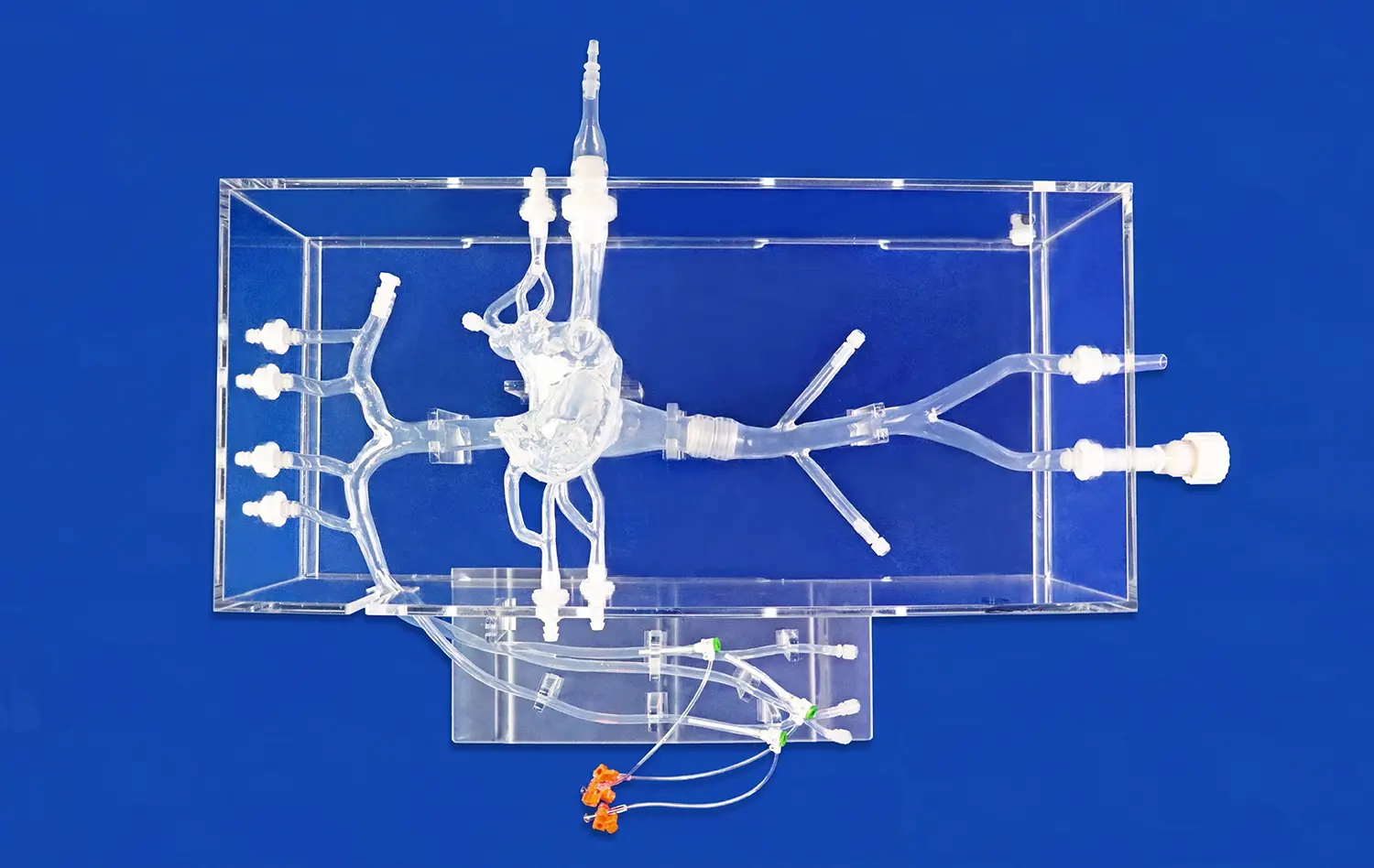
The ability to interact with a tactile representation of the patient's coronary anatomy also facilitates communication within the healthcare team. Surgeons, interventional cardiologists, and other specialists can collaboratively examine the model, discuss potential challenges, and agree on the optimal approach for each case. This multidisciplinary interaction, centered around the PCI model, often leads to more comprehensive and effective treatment strategies.
Simulating Procedural Steps and Identifying Potential Challenges
Beyond visualization, PCI models serve as invaluable tools for simulating the actual steps of a coronary intervention. Cardiologists can use these models to practice catheter navigation, gauge the feasibility of different access routes, and anticipate potential difficulties that may arise during the procedure. This hands-on rehearsal is particularly beneficial when planning interventions for complex lesions, such as chronic total occlusions (CTOs) or bifurcation lesions, where the success of the procedure often hinges on precise technique and equipment selection.
By simulating the intervention on a patient-specific model, interventionalists can identify and prepare for potential challenges before encountering them in the catheterization laboratory. This proactive approach not only enhances procedural safety but also improves efficiency, potentially reducing procedure times and minimizing radiation exposure for both patients and medical staff. Moreover, the insights gained from these simulations can inform decisions about the necessity of adjunctive imaging techniques or specialized equipment, ensuring that all required resources are available when needed.
In What Ways Do PCI Models Assist in Choosing the Right Medical Devices for Treatment?
Optimizing Stent Selection and Sizing
One of the most critical aspects of coronary interventions is the selection of appropriate stents or other implantable devices. PCI models play a crucial role in this decision-making process by allowing cardiologists to assess the dimensions and characteristics of the target vessel with unprecedented accuracy. By measuring vessel diameters, lesion lengths, and the extent of calcification on the physical model, interventionalists can make more informed choices regarding stent size, length, and type.
This precise matching of stent characteristics to patient anatomy is essential for achieving optimal procedural outcomes. Undersized stents may result in inadequate lesion coverage or stent malapposition, while oversized stents can increase the risk of vessel injury or restenosis. The ability to test different stent sizes and configurations on the PCI model before the actual procedure helps ensure that the selected devices will provide the best possible fit and functional outcome for each patient.
Evaluating Specialized Devices and Techniques
For complex coronary interventions, such as those involving bifurcations or chronic total occlusions, specialized devices and techniques are often required. PCI models provide an ideal platform for evaluating the suitability and potential efficacy of these advanced interventional tools. Cardiologists can use the models to assess whether a particular bifurcation stenting technique, such as culotte or T-stenting, is feasible given the patient's specific anatomy. Similarly, for CTO cases, the model can help in planning the approach for wire escalation or dissection re-entry techniques.
Furthermore, PCI models enable the testing of novel devices or experimental techniques in a risk-free environment. This capability is particularly valuable for evaluating emerging technologies or for cases where standard approaches may be challenging. By simulating the use of these specialized tools on a patient-specific model, interventionalists can gain confidence in their application and refine their techniques before employing them in clinical practice.
How Can PCI Models Be Used to Predict Procedural Outcomes and Complications?
Assessing Procedural Risk and Feasibility
PCI models serve as powerful tools for assessing the potential risks and feasibility of coronary interventions. By providing a detailed representation of the patient's coronary anatomy, these models allow cardiologists to evaluate the likelihood of procedural success and identify potential complications before the intervention begins. This risk assessment is particularly valuable in complex cases, such as those involving heavily calcified lesions, tortuous vessels, or multiple stenoses.
Interventionalists can use the PCI model to simulate various procedural scenarios, assessing the ease of catheter delivery, the potential for vessel perforation or dissection, and the risk of side branch occlusion in bifurcation lesions. This predictive capability enables more informed decision-making regarding the choice between percutaneous intervention and alternative treatment options, such as coronary artery bypass grafting. Moreover, it allows for better patient counseling, providing a more accurate picture of the potential benefits and risks associated with the proposed intervention.
Predicting Hemodynamic Outcomes
Advanced PCI models, when combined with computational fluid dynamics (CFD) simulations, offer the potential to predict the hemodynamic outcomes of coronary interventions. By analyzing blood flow patterns and pressure gradients within the modeled coronary arteries, cardiologists can estimate the potential improvement in coronary perfusion that may result from a planned intervention. This predictive modeling can be particularly useful in assessing the functional significance of intermediate lesions or in determining the optimal extent of revascularization in patients with multivessel disease.
Furthermore, these hemodynamic simulations can help in predicting the risk of restenosis or thrombosis following stent implantation. By examining flow patterns around proposed stent locations, interventionalists can identify areas of potential flow disturbance or stagnation that may increase the risk of adverse events. This information can guide decisions regarding stent positioning, the need for post-dilation, or the potential benefits of prolonged dual antiplatelet therapy.
Conclusion
The integration of PCI models into patient-specific planning for coronary interventions represents a significant advancement in interventional cardiology. These 3D printed simulations offer unparalleled insights into individual coronary anatomy, enabling more precise procedural planning, optimized device selection, and improved risk assessment. As the technology continues to evolve, the role of PCI models in enhancing the safety, efficacy, and personalization of coronary interventions is likely to expand further, ultimately leading to better outcomes for patients with coronary artery disease.
Contact Us
To learn more about how our advanced PCI models can revolutionize your coronary intervention planning, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to assist you in implementing this cutting-edge technology in your practice, helping you deliver the highest standard of personalized care to your patients.
References
Smith, J. et al. (2022). "Utilization of 3D Printed PCI Models in Complex Coronary Interventions: A Systematic Review." Journal of Interventional Cardiology.
Johnson, M. R. et al. (2021). "Patient-Specific 3D Models for Coronary Intervention Planning: Impact on Procedural Outcomes." Circulation: Cardiovascular Interventions.
Lee, S. H. et al. (2023). "Advanced PCI Modeling Techniques for Predicting Hemodynamic Outcomes in Coronary Interventions." European Heart Journal.
Garcia-Garcia, H. M. et al. (2022). "The Role of 3D Printed Coronary Models in Optimizing Stent Selection and Sizing." JACC: Cardiovascular Interventions.
Patel, R. A. et al. (2021). "Integration of 3D Printed PCI Models in Interventional Cardiology Training Programs: A Multi-Center Experience." Catheterization and Cardiovascular Interventions.
Wong, K. L. et al. (2023). "Cost-Effectiveness Analysis of Patient-Specific PCI Models in Complex Coronary Interventions." American Journal of Cardiology.


_1732863713705.webp)