How Do Human Blood Vessel Models Help Study Cardiovascular Diseases?
2024-11-28 16:11:51
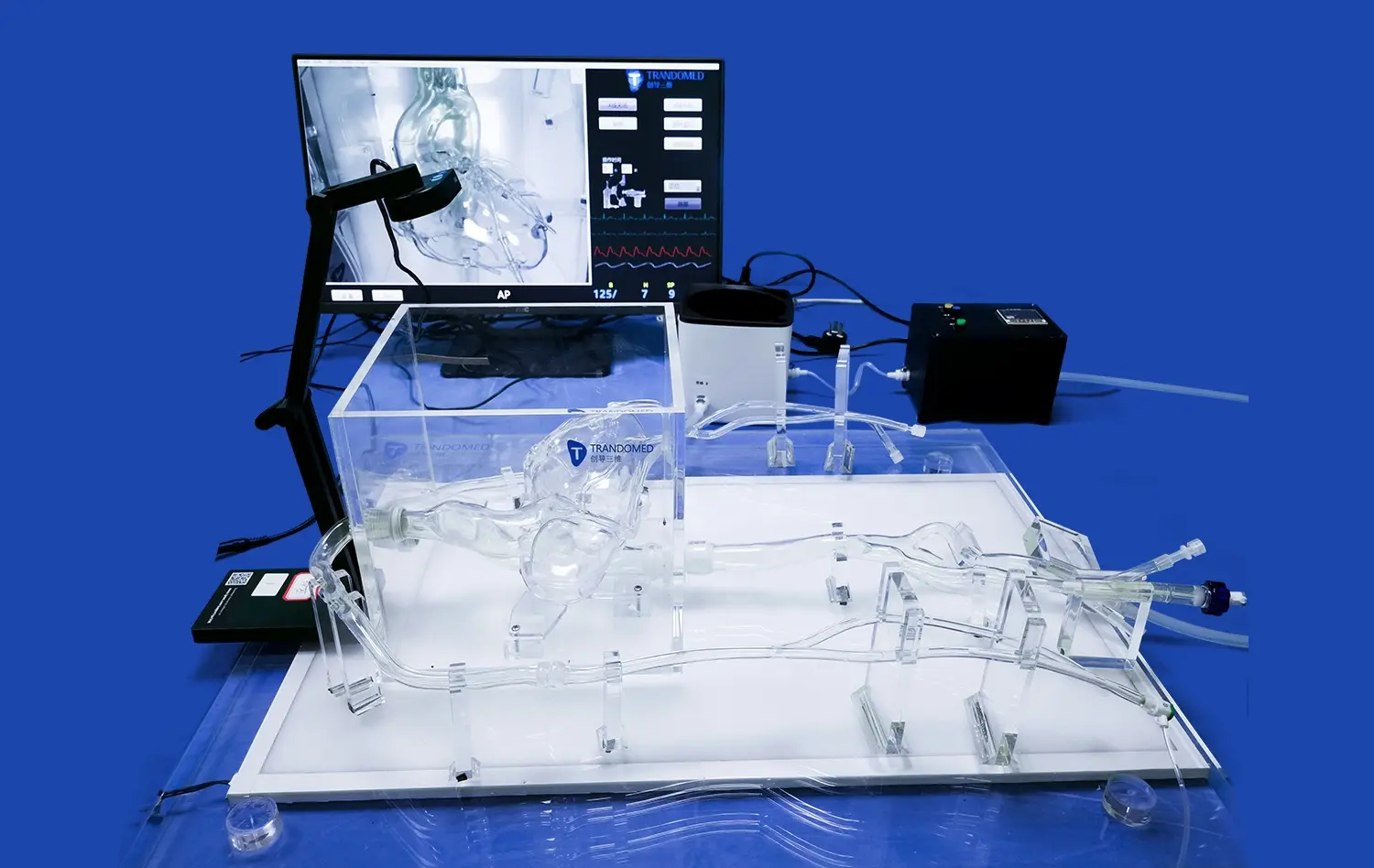
Human blood vessel models have become invaluable tools in medical research, particularly in the study of cardiovascular diseases. These models offer a realistic and highly detailed representation of human vasculature, allowing researchers to explore disease mechanisms, test treatments, and develop new diagnostic techniques in ways that were not possible before. By simulating real-life conditions, human blood vessel models help scientists understand complex cardiovascular diseases such as atherosclerosis, stroke, and clot formation. They also provide a safe, controlled environment to test non-invasive procedures, ultimately enhancing patient outcomes and reducing risks in clinical settings.
How Do Human Blood Vessel Models Advance the Study of Atherosclerosis?
Atherosclerosis, a condition characterized by the hardening and narrowing of arteries due to plaque buildup, is a leading cause of heart attacks and strokes. Human blood vessel models play a critical role in advancing our understanding of atherosclerosis by offering a lifelike simulation of arterial structures and functions. These models allow researchers to observe how plaque accumulates and grows over time, leading to the narrowing of blood vessels and restricting blood flow.
Simulating Plaque Buildup and Arterial Narrowing
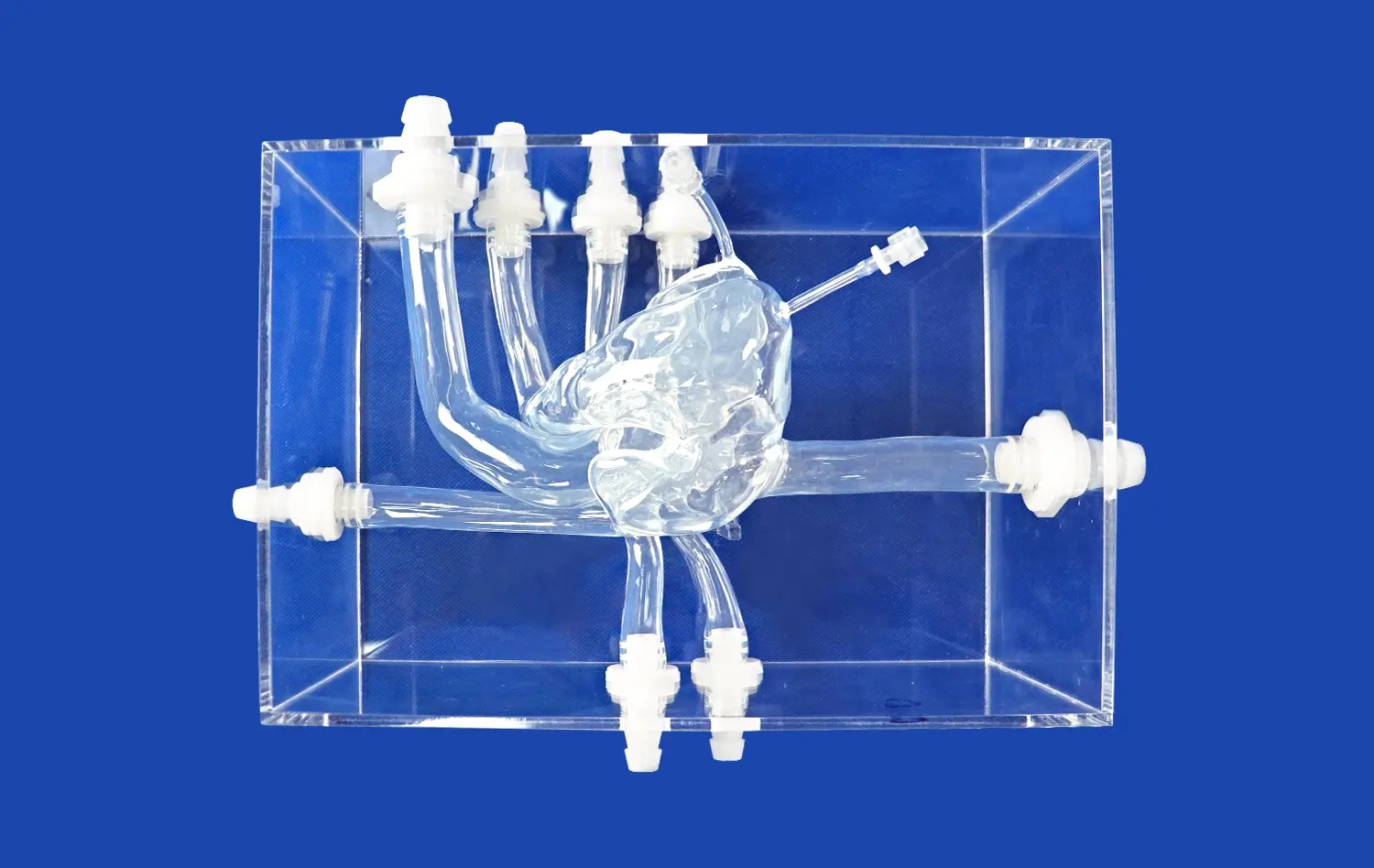
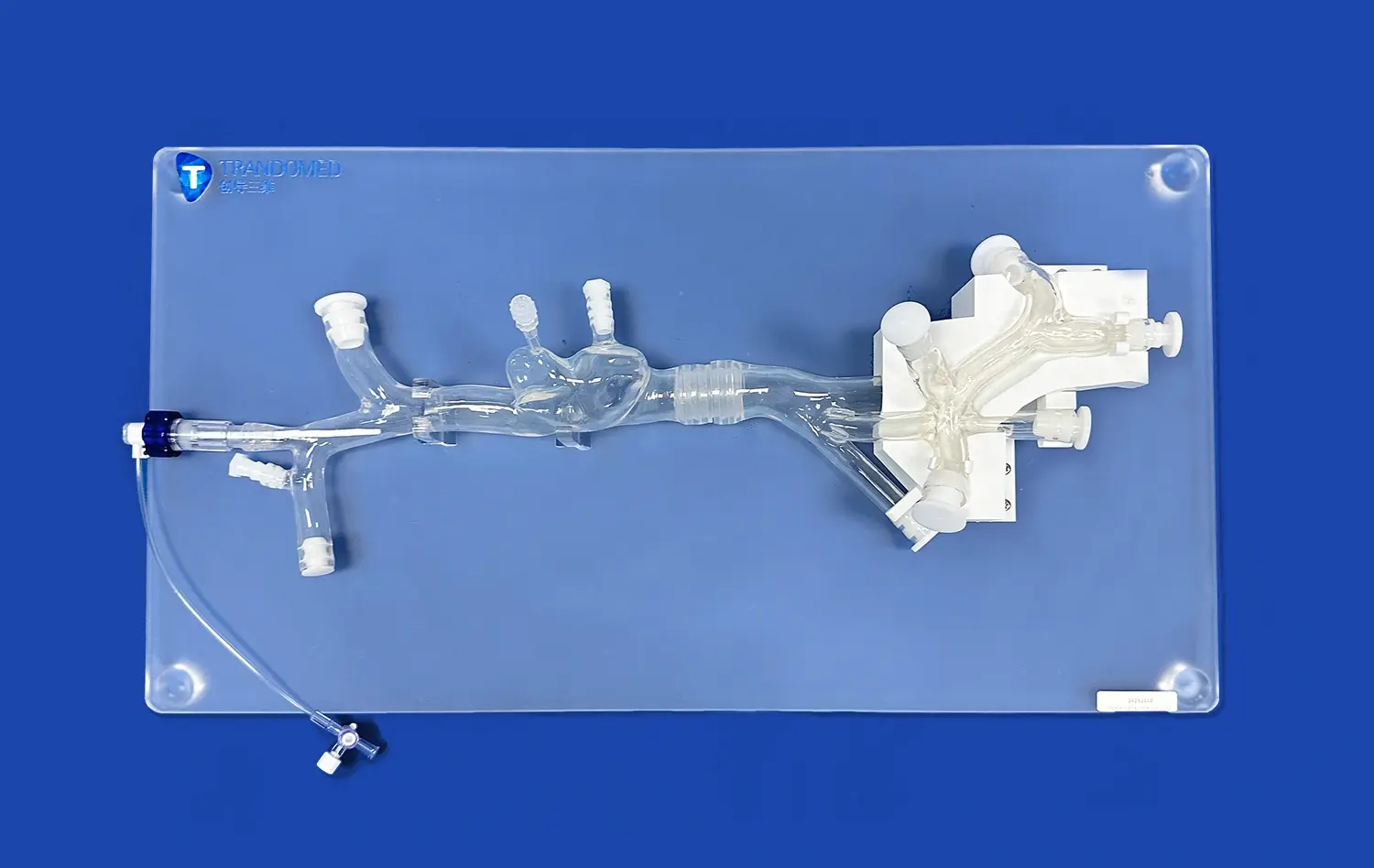
Atherosclerosis is a complex disease that develops slowly over many years. With the help of 3D-printed blood vessel models, researchers can replicate the stages of plaque accumulation and study how it impacts the elasticity and function of arterial walls. These models allow for microscopic examination of the interaction between blood flow and the vessel's inner lining, offering insights into how inflammation and lipid deposits contribute to disease progression.
Moreover, these human blood vessel models are particularly useful for testing interventions aimed at reducing plaque buildup. Researchers can simulate different treatment scenarios, and compare their efficacy in reducing plaque deposits or slowing disease progression.
Improving Surgical Planning and Risk Assessment
In addition to research, human blood vessel models are being utilized in surgical planning for cardiovascular interventions. Surgeons can use patient-specific blood vessel models to better understand the extent of arterial blockages and tailor their approach for procedures such as angioplasty or stent placement. This personalized approach helps reduce risks during surgery and improves overall outcomes for patients. By simulating real-life conditions, these models allow surgeons to practice complex surgeries in a risk-free environment, ensuring higher precision and better patient outcomes.
Can Human Blood Vessel Models Predict Outcomes of Stroke and Clot Formation?
Stroke, fundamentally caused by blood clots hindering blood stream to the brain, remains one of the most weakening cardiovascular conditions. Human blood vessel models are revolutionizing our capacity to anticipate and ponder stroke and clot arrangement, giving analysts and clinicians with a more profound understanding of how and where clots shape, and how best to avoid or treat them.
Modeling Blood Flow and Clot Dynamics
Human blood vessel models allow for the recreation of realistic blood flow dynamics, empowering analysts to watch how blood clots frame in real-time. These models can reenact distinctive conditions that lead to clot arrangement, such as changes in blood weight, vessel measure, and blood thickness. By reproducing the correct conditions beneath which clots create, analysts can superior get it the triggers for clot arrangement.
In stroke inquire about, human blood vessel models offer a special opportunity to consider ischemic strokes, which happen when blood stream to the brain is blocked by a clot. Analysts can recreate blood clot expulsion strategies, such as thrombectomy, and test modern gadgets planned to extricate clots more effectively.
Assessing Stroke Risk and Treatment Efficacy
Human blood vessel models are also used in predictive modeling for stroke risk assessment. By analyzing patient-specific data, such as blood pressure and cholesterol levels, researchers can create personalized models that help predict an individual's likelihood of experiencing a stroke. These models allow for the testing of preventive measures and early interventions, such as lifestyle changes, in a highly controlled environment.
Furthermore, these models are helping clinicians refine post-stroke recovery strategies by allowing them to simulate different rehabilitation approaches. For example, they can test how various therapies, such as physical therapy or blood pressure management, might impact recovery outcomes after a stroke.
How Do Human Blood Vessel Models Advance Non-Invasive Diagnostic Techniques?
With progressions in restorative innovation, there is a developing accentuation on non-invasive symptomatic strategies for cardiovascular infections. Human blood vessel models are playing a pivotal part in the improvement and refinement of these strategies, advertising a viable and moral way to test and progress strategies without the require for intrusive methods or creature testing.
Enhancing Imaging and Diagnostic Technologies
Non-invasive techniques such as ultrasound, MRI, and CT scans rely on accurate imaging of blood vessels to diagnose cardiovascular diseases. Human blood vessel models provide an ideal platform for testing and optimizing these imaging technologies. The highly realistic nature of these models allows researchers to fine-tune imaging settings to improve clarity and accuracy when detecting issues like arterial blockages, aneurysms, or plaque buildup, thereby enhancing early detection of cardiovascular diseases.
By utilizing 3D-printed human blood vessel models, analysts can mimic different pathologies such as limited courses or aneurysms and watch how these conditions show up in diverse imaging modalities. This makes a difference radiologists and restorative specialists fine-tune their symptomatic instruments and strategies, making it simpler to spot early signs of infection in genuine patients. Moreover, these models permit for testing modern imaging conventions or program calculations, guaranteeing that non-invasive demonstrative strategies are as exact and compelling as conceivable.
Testing Non-Invasive Treatment Methods
Beyond diagnostics, human blood vessel models are also helping to advance non-invasive treatment methods. For example, techniques such as focused ultrasound or laser-based therapies are being developed to treat specific cardiovascular conditions without the need for surgery. Researchers can use these models to test the effectiveness and safety of these emerging therapies, ensuring that they target problem areas precisely without damaging surrounding tissues.
By recreating real-life blood stream and vessel structures, these models give profitable experiences into how non-invasive treatments connected with the cardiovascular framework. This empowers analysts to refine these strategies and make them more secure and more successful some time recently they are utilized in clinical settings.
Conclusion
Human blood vessel models are transforming the study and treatment of cardiovascular diseases by providing detailed, realistic simulations of the human vascular system. From advancing the understanding of atherosclerosis and improving stroke treatment to enhancing non-invasive diagnostic techniques, these models are playing a critical role in modern medical research and clinical practice. By offering a safer, more ethical, and highly controlled environment for testing, human blood vessel models are driving significant improvements in both patient outcomes and the development of innovative treatments.
Contact Us
If you're interested in learning more about our advanced 3D printed silicone medical simulators, including our state-of-the-art human blood vessel models, we invite you to contact us. Our team at Trandomed is dedicated to providing cutting-edge solutions for medical research and education. Reach out to us at jackson.chen@trandomed.com to discuss how our products can enhance your cardiovascular research or medical training programs.
References
Libby, P. (2021). Inflammation in Atherosclerosis: From Pathophysiology to Practice. Journal of the American College of Cardiology.
Prabhakaran, S., Ruff, I., & Bernstein, R. A. (2015). Stroke: Mechanisms, Diagnosis, and Management. Journal of Clinical Neurology.
Virmani, R., Burke, A. P., Farb, A., & Kolodgie, F. D. (2006). Pathology of the Vulnerable Plaque. Journal of the American College of Cardiology.
Goyal, M., Menon, B. K., van Zwam, W. H., et al. (2016). Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. The Lancet.
Fuster, V., Badimon, L., & Badimon, J. J. (1992). The Pathogenesis of Coronary Artery Disease and the Acute Coronary Syndromes. The New England Journal of Medicine.
Adams, H. P., Bendixen, B. H., Kappelle, L. J., et al. (1993). Classification of Subtypes of Acute Ischemic Stroke: Definitions for Use in a Multi-Center Clinical Trial. Stroke.