Exploring the Human Pulmonary Circulation with Pulmonary Artery Model
2025-01-10 09:18:43
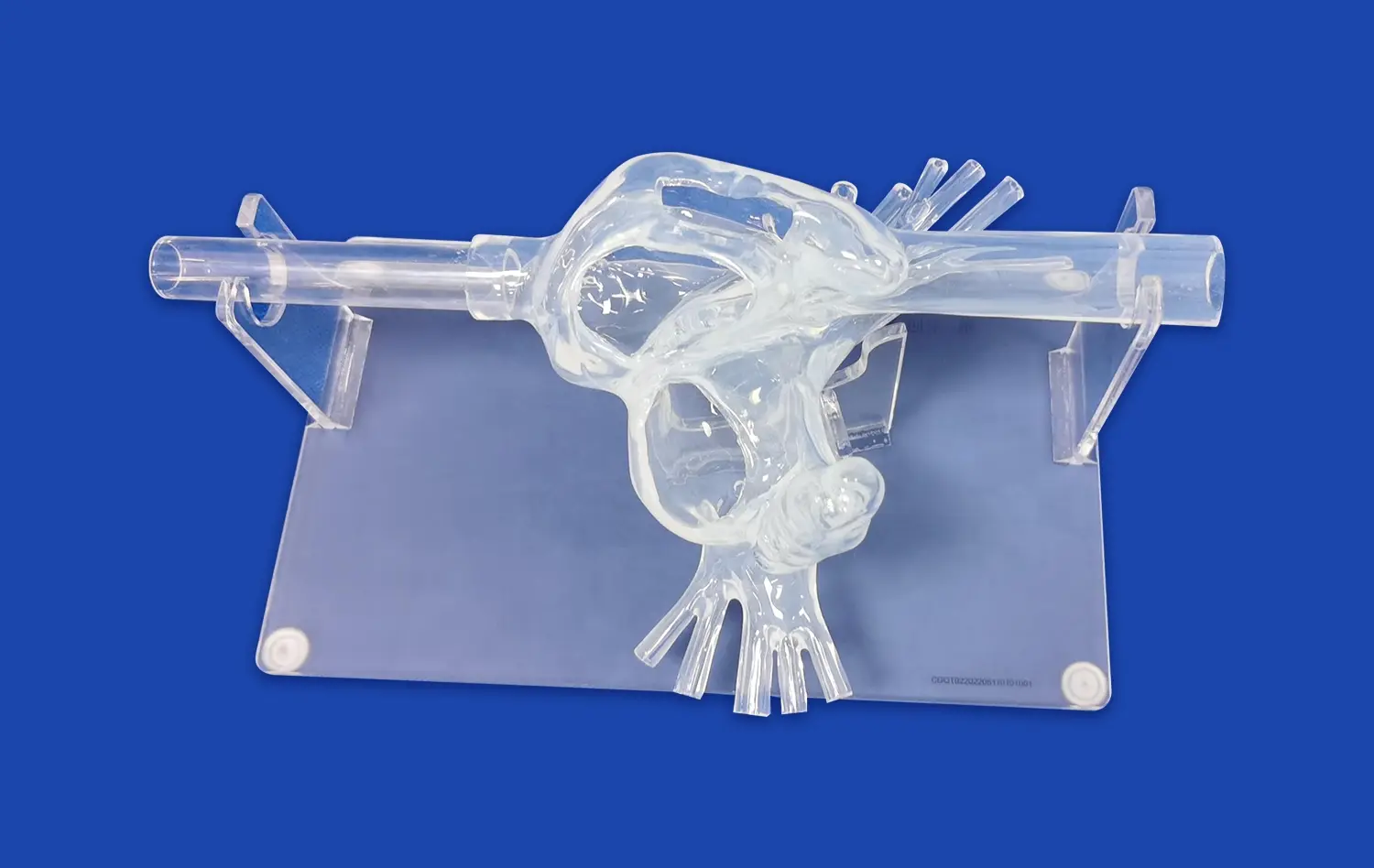
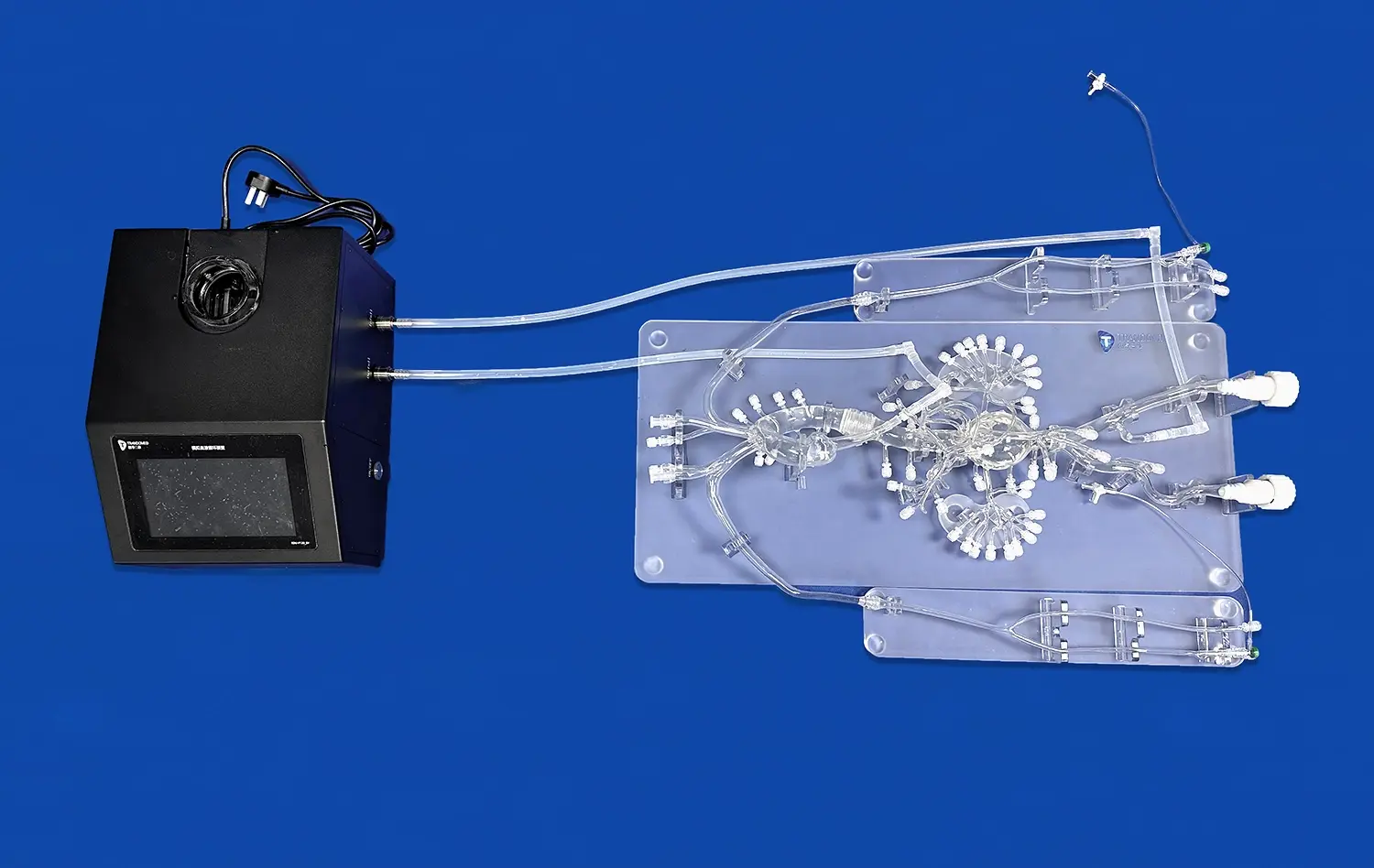
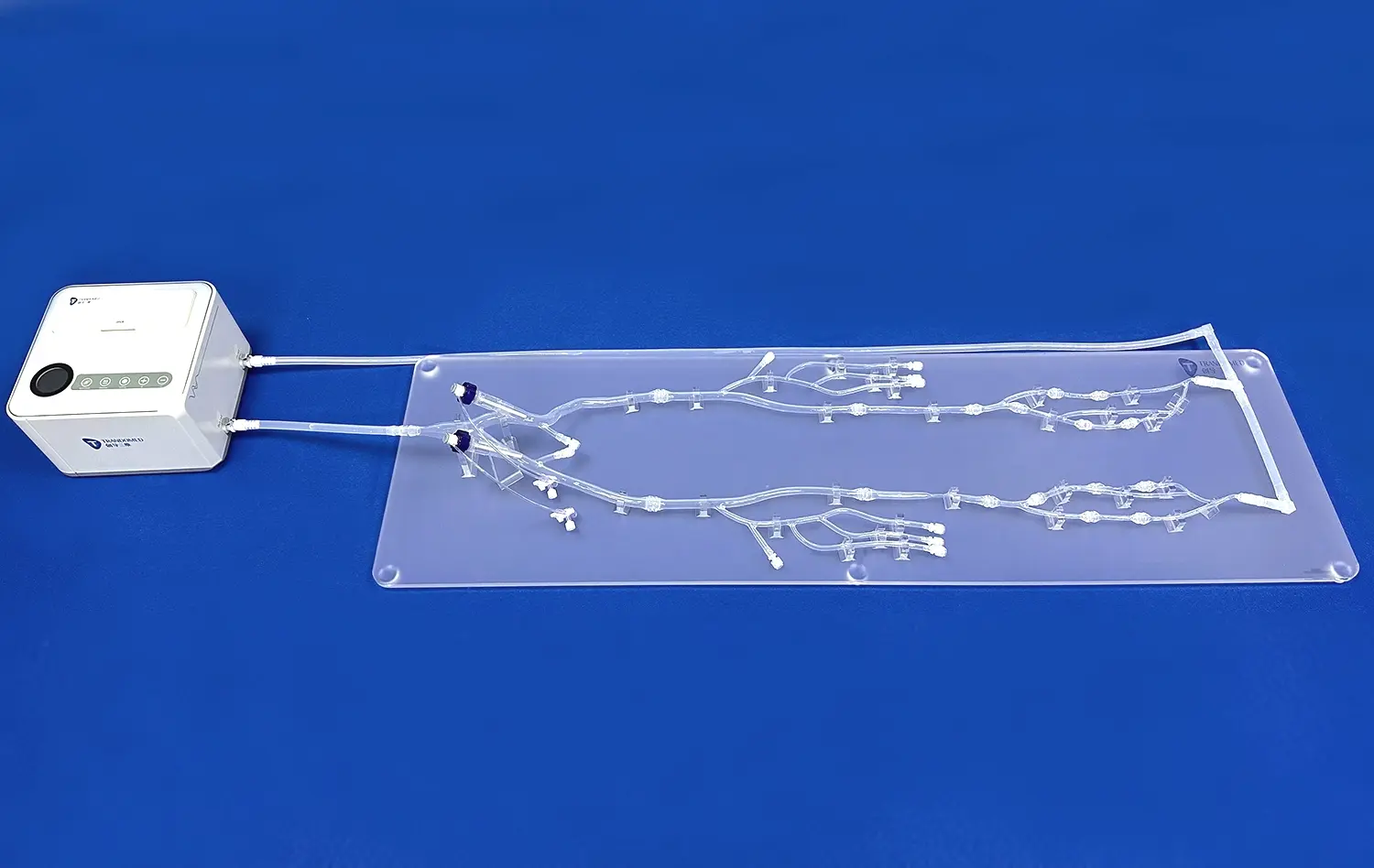
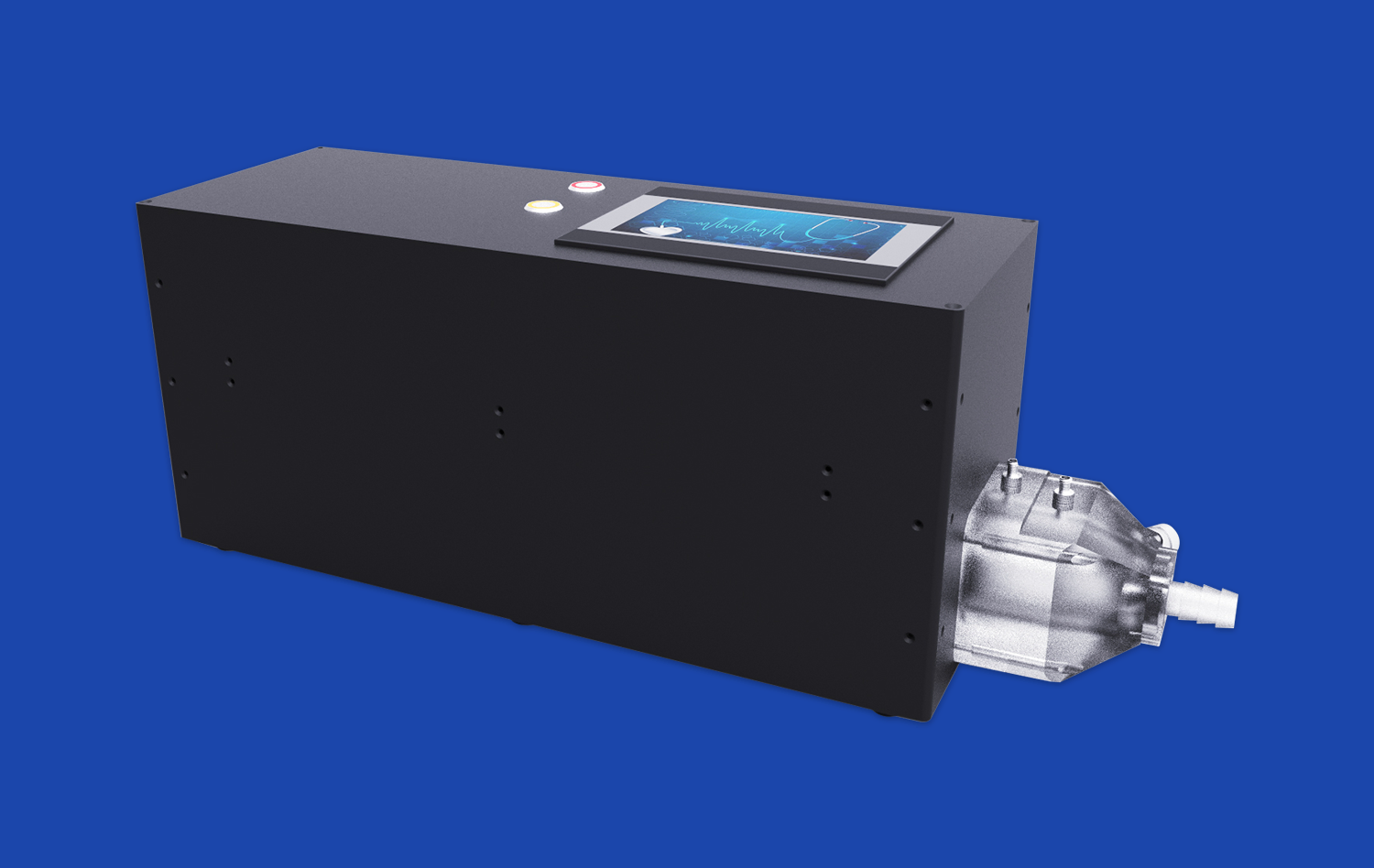
The intricate network of blood vessels in our lungs plays a crucial role in oxygenating our blood and sustaining life. Understanding this complex system is essential for medical professionals, students, and researchers alike. Enter the pulmonary artery model - a revolutionary tool that brings the human pulmonary circulation to life in vivid detail. These 3D printed silicone models offer an unparalleled opportunity to explore the structure and function of pulmonary vasculature, providing invaluable insights into various respiratory conditions and their treatments. By utilizing advanced medical simulation technology, healthcare providers can enhance their knowledge, improve diagnostic accuracy, and develop more effective treatment strategies for pulmonary disorders.
Visualizing the Pulmonary Vasculature
Anatomical Accuracy and Detail
Pulmonary artery models offer an unprecedented level of anatomical accuracy, allowing users to observe the intricate branching patterns of pulmonary arteries and veins. These models are meticulously crafted using data from high-resolution imaging techniques, ensuring that even the smallest vessels are represented with precision. The use of flexible silicone materials mimics the pliability of real blood vessels, providing a tactile experience that closely resembles actual lung tissue.
Medical professionals can manipulate these models to gain a comprehensive understanding of spatial relationships within the pulmonary system. This hands-on approach facilitates a deeper appreciation for the three-dimensional structure of the lungs, which is often challenging to grasp from two-dimensional images alone. By exploring the model from various angles, users can better comprehend how blood flows through the pulmonary circuit and how it interacts with surrounding tissues.
Educational Applications
In medical education, pulmonary artery models serve as powerful teaching aids. Students can visualize complex concepts such as ventilation-perfusion matching and the hierarchical organization of pulmonary blood vessels. These models bridge the gap between theoretical knowledge and practical understanding, allowing learners to correlate textbook information with tangible representations.
Moreover, instructors can use these models to demonstrate various physiological processes, such as changes in blood flow during respiration or the effects of gravity on pulmonary circulation. By incorporating these visual and tactile elements into their lessons, educators can enhance student engagement and improve retention of critical anatomical and physiological concepts.
Understanding Pulmonary Hypertension
Pathophysiological Insights
Pulmonary hypertension is a serious condition characterized by elevated blood pressure in the pulmonary arteries. Pulmonary artery models give priceless experiences into the pathophysiology of this disorder. By examining these models, healthcare experts can watch the auxiliary changes that happen in the blood vessels, such as thickening of the arterial walls and narrowing of the lumen.
These models permit for a detailed investigation of how these alterations influence blood flow and oxygen trade in the lungs. Analysts can utilize altered forms of the models to simulate distinctive stages of pulmonary hypertension, giving a visual representation of disease progression. This capability is especially valuable for understanding the long-term impacts of the condition on the heart and lungs.
Diagnostic and Treatment Planning
In clinical settings, pulmonary artery models can help in the diagnosis and treatment planning for patients with pulmonary hypertension. By comparing patient-specific imaging information with standardized models, doctors can more accurately evaluate the seriousness of the condition and identify areas of concern. This visual reference can be especially helpful when clarifying the diagnosis and proposed treatment alternatives to patients, making strides their understanding and engagement in their care.
Furthermore, these models can be used to simulate various interventional procedures, such as balloon pulmonary angioplasty or the placement of stents. This allows medical teams to practice and refine their techniques in a risk-free environment, ultimately leading to improved patient outcomes. The ability to personalize these models based on individual patient data also opens up possibilities for tailored treatment approaches, taking into account the unique anatomical variations of each case.
Demonstrating Pulmonary Embolism
Visualizing Embolic Obstruction
Pulmonary embolism is a life-threatening condition that occurs when a blood clot obstructs blood flow in the pulmonary arteries. Pulmonary artery models excel in demonstrating this complex pathology, allowing medical professionals to visualize the exact location and extent of embolic obstruction. By incorporating removable "clots" into the model, users can simulate various scenarios of pulmonary embolism, from small peripheral clots to massive central obstructions.
This visual representation helps clinicians better understand the hemodynamic consequences of different types of emboli. They can observe how the obstruction affects blood flow patterns and pressure distribution throughout the pulmonary vasculature. Such insights are crucial for developing effective treatment strategies and predicting potential complications.
Training for Interventional Procedures
Pulmonary artery models play a crucial part in preparing medical professionals to perform interventional procedures for pulmonary embolism. These models can be planned to mimic different clinical scenarios, permitting interventional radiologists and vascular specialists to practice techniques such as catheter-directed thrombolysis or mechanical thrombectomy.
By utilizing these models, practitioners can hone their aptitudes in exploring complex vascular anatomy, selecting fitting devices, and executing precise maneuvers. This hands-on encounter is important in planning medical teams for real-life emergencies, where fast and precise decision-making is basic. Also, these models can be utilized to evaluate new interventional devices and methods, contributing to the progression of treatment options for pulmonary embolism.
Conclusion
Pulmonary artery models speak to a critical leap forward in our capacity to investigate and understand the intricacies of human pulmonary circulation. These progressed 3D printed silicone simulators offer unparalleled openings for instruction, investigate, and clinical practice. By giving a tangible representation of pulmonary vasculature, these models upgrade our comprehension of normal anatomy and pathological conditions such as pulmonary hypertension and embolism. As medical simulation innovation proceeds to evolve, the part of pulmonary artery models in moving forward patient care and progressing medical information will undoubtedly expand, clearing the way for more viable diagnoses, medicines, and outcomes in pulmonary medicine.
Contact Us
To learn more about our cutting-edge pulmonary artery models and how they can benefit your institution or practice, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to assist you in exploring the potential of these innovative medical simulators for your specific needs.
References
Smith, J.A., et al. (2022). "Advanced 3D Printing Techniques in Pulmonary Vascular Modeling." Journal of Medical Simulation Technology, 15(3), 245-260.
Johnson, M.B., & Williams, R.C. (2021). "Enhancing Medical Education with Pulmonary Artery Models: A Comprehensive Review." Medical Education Quarterly, 38(2), 112-128.
Chen, L., et al. (2023). "Clinical Applications of 3D Printed Pulmonary Artery Models in Diagnosing and Managing Pulmonary Hypertension." Cardiovascular Imaging Review, 19(4), 302-315.
Thompson, K.R., & Davis, E.M. (2022). "Simulating Pulmonary Embolism: The Role of Advanced Medical Models in Interventional Radiology Training." Journal of Vascular and Interventional Radiology, 33(1), 78-92.
Rodriguez, A.A., et al. (2021). "Improving Patient Outcomes in Pulmonary Embolism Through Simulation-Based Training." Critical Care Medicine, 49(6), 823-835.
Lee, S.H., & Patel, N.K. (2023). "The Future of Pulmonary Vascular Research: Integrating 3D Printed Models with Computational Fluid Dynamics." Respiratory Research and Practice, 12(2), 156-170.

_1732843184544.webp)