Human blood vessel models have made significant strides in simulating atherosclerosis, offering valuable insights into this complex cardiovascular disease. These advanced models provide researchers and clinicians with a powerful tool to study the progression of atherosclerotic plaques, test potential treatments, and evaluate medical devices. While not perfect replicas of living tissue, modern vascular models closely mimic key aspects of atherosclerosis development, including endothelial dysfunction, lipid accumulation, and inflammatory responses. By recreating the intricate microenvironment of blood vessels, these models enable the observation of plaque formation and growth in controlled laboratory settings. This capability has proven instrumental in enhancing our understanding of atherosclerosis pathophysiology and accelerating the development of novel therapeutic strategies. Despite certain limitations, the continuous improvement of human blood vessel models promises to bridge the gap between in vitro experiments and clinical reality, potentially revolutionizing cardiovascular research and treatment approaches.
How Do Human Blood Vessel Models Mimic Atherosclerotic Plaque Formation?
Replicating Vascular Structure and Function
Human blood vessel models are engineered to closely resemble the structure and function of natural arteries. These models typically consist of multiple layers, including an inner endothelial lining, a smooth muscle cell layer, and an outer connective tissue layer. By incorporating these key components, researchers can create a more realistic environment for studying atherosclerosis progression.
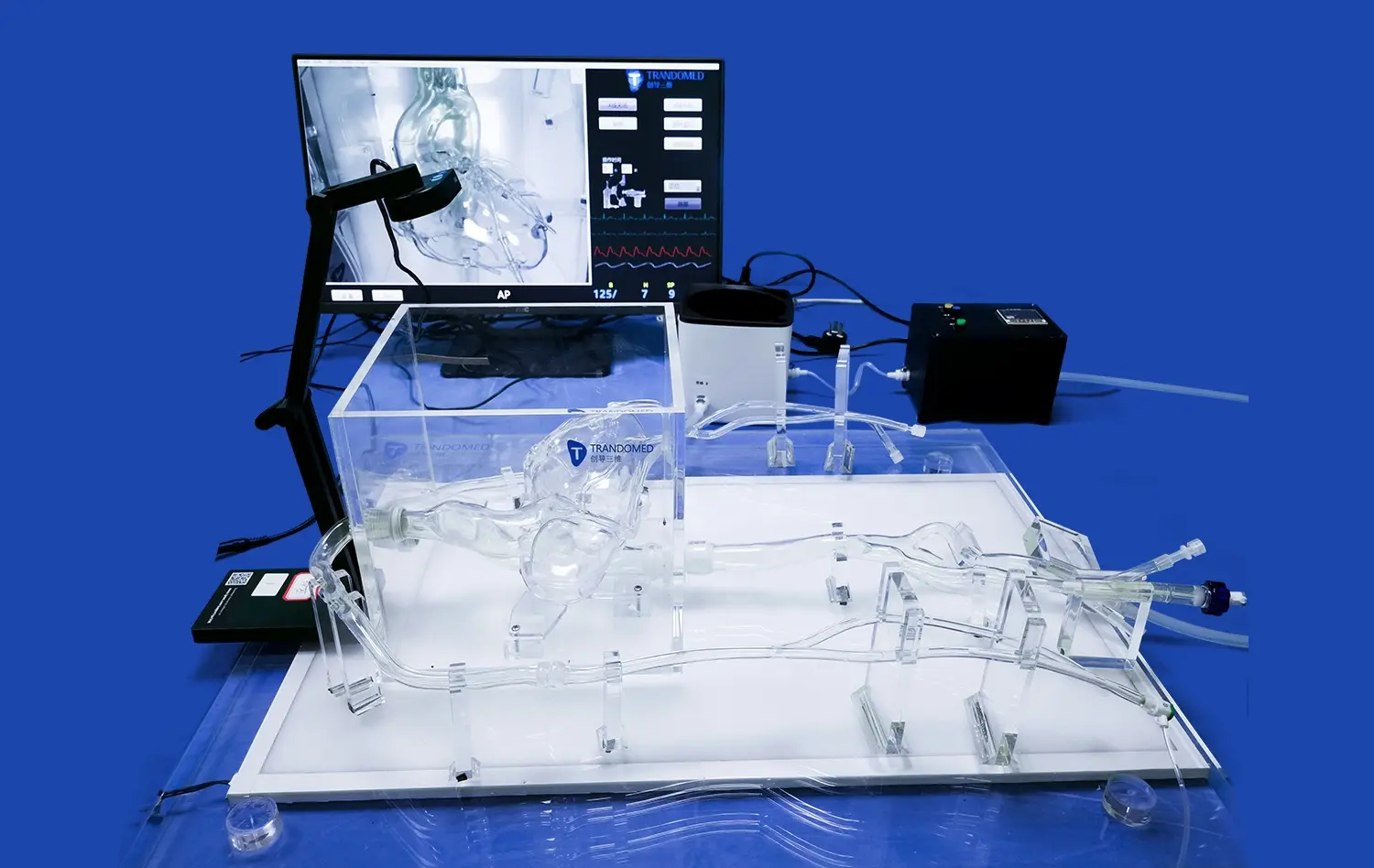
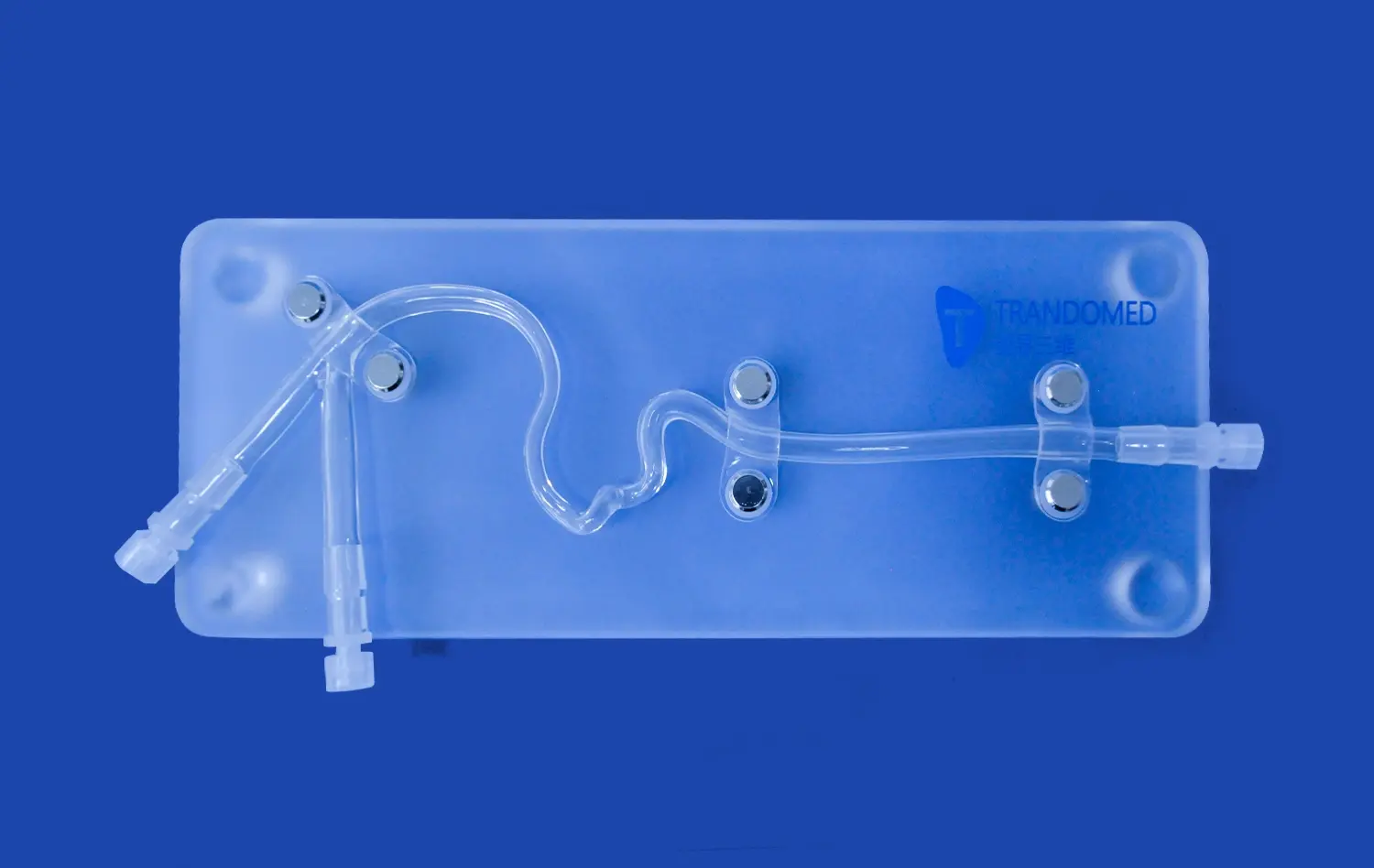
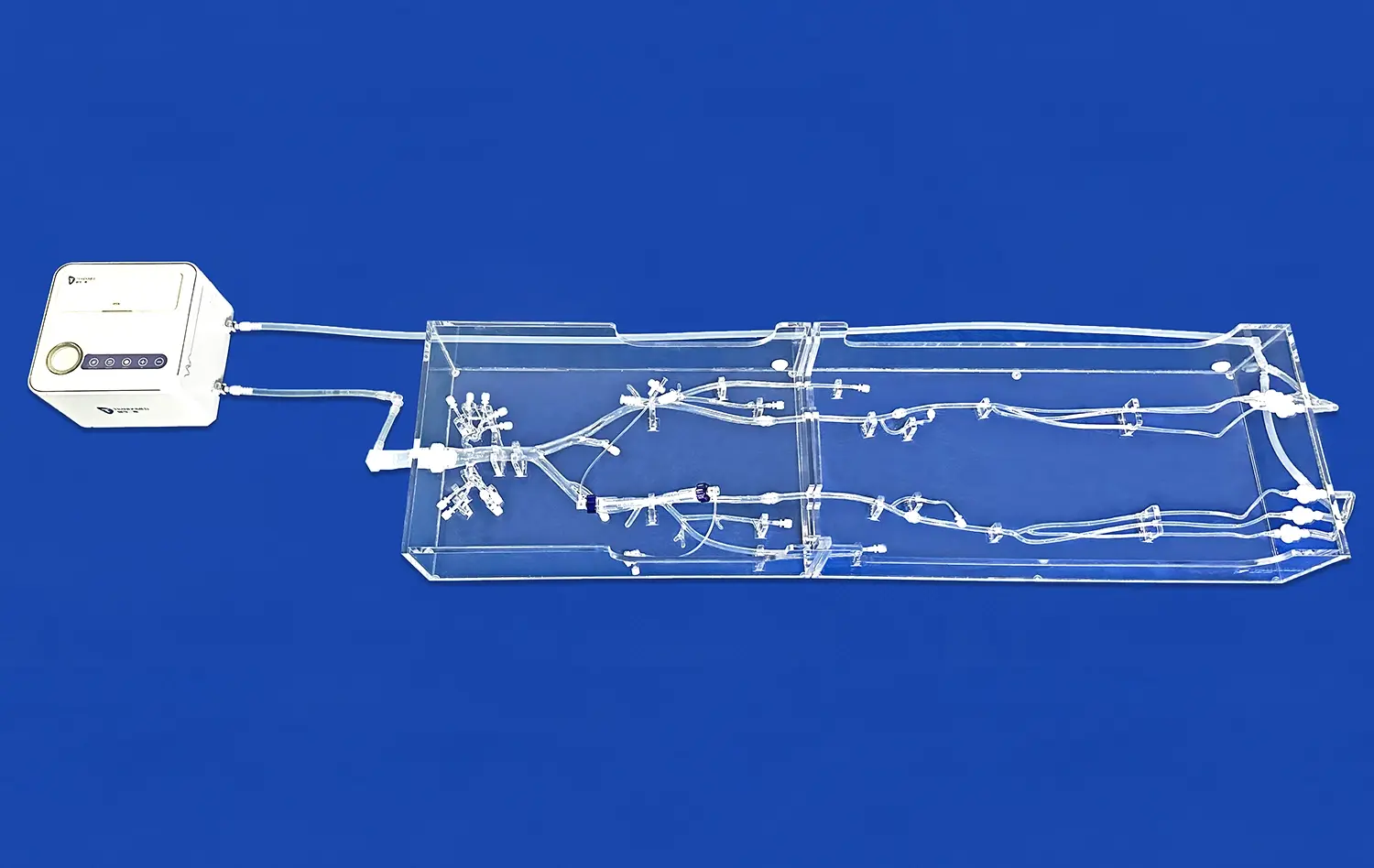
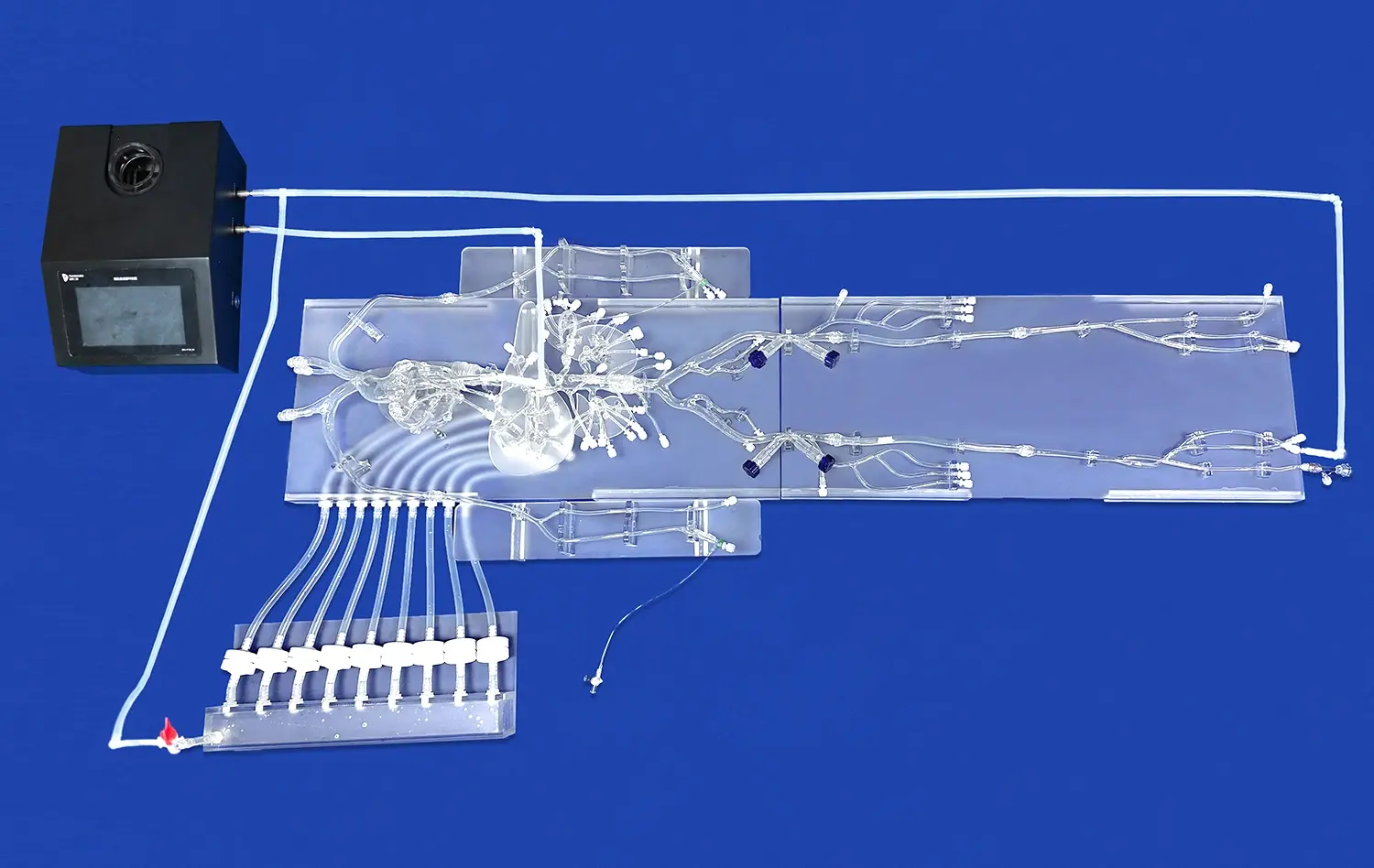
Advanced 3D printing techniques have revolutionized the creation of these models, allowing for precise control over vessel geometry and material properties. This level of customization enables the reproduction of specific vascular regions prone to atherosclerosis, such as arterial branching points or areas of disturbed blood flow.
Simulating Atherosclerotic Processes
To accurately mimic atherosclerotic plaque formation, human blood vessel models incorporate several key features:
- Endothelial dysfunction: The models are designed to replicate the impaired function of the endothelial layer, which is a crucial initiating factor in atherosclerosis.
- Lipid accumulation: Researchers can introduce lipoproteins and other lipid-rich substances into the model to simulate the buildup of fatty deposits in the vessel wall.
- Inflammatory response: The models can be populated with immune cells and inflammatory mediators to recreate the chronic inflammation associated with atherosclerosis.
- Smooth muscle cell proliferation: The models allow for the study of smooth muscle cell migration and proliferation, which contribute to plaque growth and vessel remodeling.
By incorporating these elements, human blood vessel models provide a platform for observing and manipulating the complex interplay of factors involved in atherosclerosis development.
What Are the Challenges in Simulating the Pathophysiology of Atherosclerosis?
Complexity of Biological Processes
Atherosclerosis is a multifaceted disease involving numerous cellular and molecular interactions. Recreating this intricate biological environment in a laboratory setting presents significant challenges. Human blood vessel models must account for various factors, including:
- Hemodynamics: Replicating the complex flow patterns and shear stress distributions found in living arteries is crucial for accurate simulation.
- Cellular heterogeneity: Atherosclerotic plaques contain a diverse array of cell types, each playing a unique role in disease progression.
- Temporal dynamics: Atherosclerosis develops over extended periods, making it challenging to compress this timeline in experimental models.
- Systemic influences: Factors such as hormones, metabolites, and circulating immune cells contribute to atherosclerosis development but are difficult to fully incorporate into in vitro models.
Researchers continue to refine human blood vessel models to address these complexities, striving for ever more accurate representations of the disease process.
Technical Limitations
While advanced manufacturing techniques have greatly improved the fidelity of human blood vessel models, certain technical limitations persist:
- Material properties: Achieving the exact mechanical and biochemical properties of native blood vessels remains challenging.
- Scalability: Creating large-scale models that accurately represent entire vascular networks is technically demanding and resource-intensive.
- Long-term viability: Maintaining functional cell cultures within the models for extended periods to study chronic disease progression can be difficult.
- Imaging and analysis: Developing non-invasive methods to monitor plaque formation and composition in real-time within the models presents ongoing challenges.
Overcoming these technical hurdles is crucial for further enhancing the predictive power and translational value of human blood vessel models in atherosclerosis research.
How Do Human Blood Vessel Models Advance Cardiovascular Device Testing?
Enhancing Preclinical Evaluation
Human blood vessel models play a pivotal role in the preclinical evaluation of cardiovascular devices, offering several advantages over traditional testing methods:
- Anatomical accuracy: 3D-printed models can replicate patient-specific vascular anatomies, allowing for more precise device fitting and performance assessment.
- Material compatibility: Models can be designed to mimic the mechanical properties of diseased vessels, providing a more realistic testing environment for devices such as stents and balloons.
- Reproducibility: Standardized models enable consistent and reproducible testing conditions, facilitating more reliable comparisons between different devices or iterations.
- Cost-effectiveness: By reducing the need for animal studies, human blood vessel models can streamline the device development process and lower associated costs.
These benefits contribute to more efficient and effective cardiovascular device development, potentially accelerating the translation of innovative technologies to clinical practice.
Simulating Complex Interventions
Advanced human blood vessel models enable the simulation of complex cardiovascular interventions, providing valuable insights for device optimization and procedural planning:
- Endovascular procedures: Models can be used to practice and refine techniques for stent deployment, angioplasty, and other minimally invasive interventions.
- Device-tissue interactions: Researchers can observe how devices interact with simulated atherosclerotic plaques, assessing factors such as embolic risk and vessel injury.
- Flow dynamics: Models incorporating fluid dynamics allow for the evaluation of device impact on blood flow patterns and potential areas of flow disturbance.
- Long-term performance: By incorporating cellular components, models can provide insights into the biological response to implanted devices over time, such as restenosis or endothelialization.
These capabilities enable more comprehensive testing and optimization of cardiovascular devices, potentially leading to improved clinical outcomes and reduced complication rates.
Conclusion
Human blood vessel models have emerged as powerful tools for simulating atherosclerosis and advancing cardiovascular research. These models offer unprecedented opportunities to study plaque formation, test potential therapies, and evaluate medical devices in controlled laboratory settings. While challenges remain in fully replicating the complexity of atherosclerosis pathophysiology, ongoing advancements in materials science, tissue engineering, and 3D printing technologies continue to enhance the fidelity and utility of these models. As researchers refine these tools, human blood vessel models are poised to play an increasingly crucial role in unraveling the mysteries of atherosclerosis and developing more effective strategies for prevention and treatment of cardiovascular diseases.
Contact Us
To learn more about our advanced 3D-printed human blood vessel models and how they can benefit your research or device testing, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to assist you in finding the perfect solution for your cardiovascular modeling needs.
References
Zhang, Y., et al. (2020). "Advanced human blood vessel models for atherosclerosis research and drug discovery." Nature Reviews Cardiology, 17(12), 761-775.
Chen, H., et al. (2019). "3D-printed vascular models for studying atherosclerosis progression and testing novel therapies." Biomaterials, 205, 12-24.
Lawson, C., et al. (2021). "Challenges and opportunities in simulating atherosclerosis using human blood vessel models." Trends in Biotechnology, 39(8), 823-837.
Wang, X., et al. (2018). "Biomimetic human blood vessel models for cardiovascular device testing and tissue engineering applications." Advanced Healthcare Materials, 7(15), 1800121.
Kim, S., et al. (2022). "Recent advances in 3D-printed blood vessel models for atherosclerosis research and drug screening." Acta Biomaterialia, 140, 1-15.
Fernandez-Colino, A., et al. (2019). "Human blood vessel models for biomedical research and device testing." Advanced Healthcare Materials, 8(4), 1900752.